Mitigating biotin interference on immunoassays is a critical factor to ensure appropriate diagnosis and treatment. There are many ways labs can reduce biotin interference.
By Tyler Radke, MLS(ASCP)CM
One-Sentence Summary:
Biotin supplementation, while beneficial for certain health conditions, can interfere with laboratory immunoassays, potentially leading to inaccurate diagnostic results due to its impact on biotin-streptavidin interactions.
Three Brief Takeaways:
- Biotin Interference: High doses of biotin can disrupt immunoassays, causing falsely elevated or reduced lab results.
- Risk Factors: Patients on high-dose biotin supplements or with renal insufficiency are most susceptible to interference.
- Mitigation Strategies: Accurate lab testing relies on clinicians being aware of biotin intake and adjusting timing or withholding supplementation accordingly.
Laboratory testing is a cornerstone of medical diagnostics, providing crucial information for the diagnosis, monitoring, and treatment of various health conditions. However, many tests can be significantly influenced by various factors throughout the testing process. Influencing factors occurring upstream of the analytic testing phase are known as preanalytical factors.
Preanalytical factors can result in false results, interpretation, or diagnosis. It is therefore critical that laboratories ensure the accuracy and reliability of their tests through the preanalytical phases.
Preanalytical factors may constitute biological aspects of the sample (lipids, bilirubin, proteins) as well as those exogenous factors, including drugs, anticoagulants, infusions, supplements, and more. Labs are familiar with those critical preanalytical factors like hemolysis, icterus, lipemia, IV contamination, and storage/transport degradation. Just as important, however, is the less commonly discussed interfering factor of biotin supplementation.
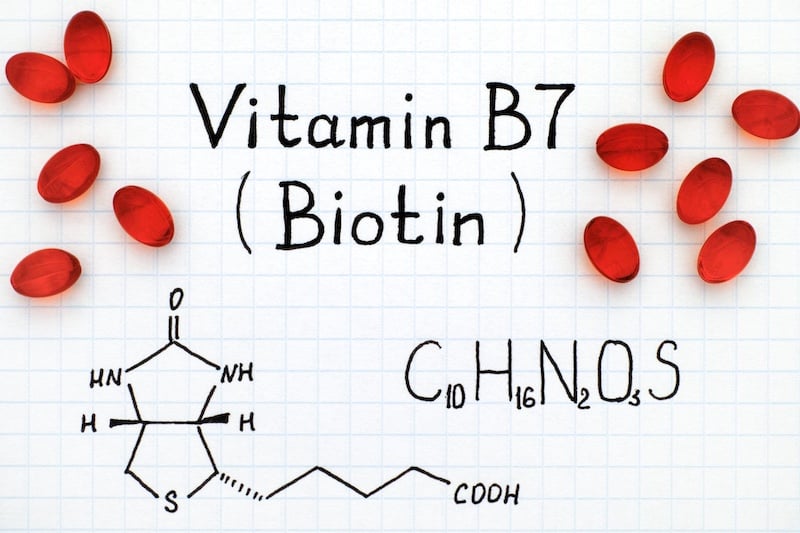
What is biotin?
Biotin, also known as vitamin B7, is a water-soluble vitamin. Biotin is essential for various metabolic processes and is recommended as a supplement for individuals with biotin deficiencies.
Biotin also plays a critical role in energy production by aiding in the metabolism of carbohydrates, fats, and proteins. Furthermore, it contributes to the maintenance of normal neurological functions and improves glucose utilization in the body, potentially aiding individuals with diabetes.
Who needs biotin?
Biotin deficiency is rare, presenting with symptoms of hair loss, brittle nails, skin rashes, and neurological issues. Biotin supplementation is beneficial for individuals with certain genetic disorders, and those undergoing prolonged parenteral nutrition who may lack adequate biotin intake. It may also be beneficial for pregnant and breastfeeding women.
It is estimated that the average biotin intake from foods such as beef, tuna, spinach, milk, bananas, and other foods results in intake ranges from 35–70 mcg/day. Meanwhile, the recommended daily adult value according to the National Institutes of Health is 25–35 mcg/day. Given this surplus, it is not surprising that biotin deficiency is rare among healthy adults. This surplus is also increased in daily life thanks to biotin’s purported health benefits, such as improving hair, skin, and nail health, leading to its inclusion in many common dietary supplements.
Multi & prenatal vitamins can contain 30-150 mcg of biotin, while supplements often packaged as hair and nail beauty treatments can contain up to 2,000-10,000 mcg of biotin.
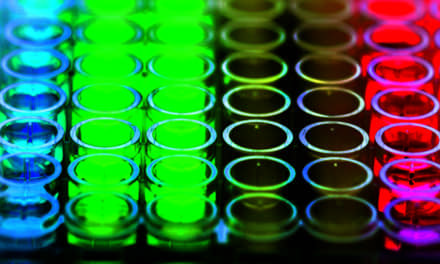
Immunoassays and Biotin Interference
This surplus can have a downside. High levels of biotin in the blood as experienced with supplementation can interfere with laboratory tests, particularly immunoassays. Many automated immunoassays use biotin-streptavidin binding as a critical step in measuring target analyte. Generally, patient sample is added to a sample well followed by the addition of a biotinylated antibody. The biotinylated antibody complexes with patient antigen, forming a biotinylated antigen/antibody complex. A subsequent step adds streptavidin to bind to the biotin complex, typically culminating in a detection process like immobilization, electrochemiluminescence, immunofluorescence, etc.
Biotin-streptavidin is used in many clinical assays due to the strong affinity and precision of this interaction, increasing test sensitivity and specificity. However, excess biotin in the blood can saturate the sample, interfering with biotin-streptavidin bonding in the assay. This interference is particularly problematic in tests for hormones, cardiac markers, and infectious diseases, where accurate measurements are crucial for clinical decision-making.
Complicating interpretation, biotin interference can generate both falsely increased or decreased results, depending on the methodology used in the test.
Biotin metabolism
Biotin plasma concentrations are known to peak within 1-2 hours of dose, with a serum clearance time of about 8 hours in healthy patients. However, biotin supplementation accumulates within the body until a steady state is achieved, around 3 days. For patients taking mega-doses of biotin, the half-life can be up to 18 hours. Patient physiologic renal status impacts biotin steady state, half-life, and wash-out period.
What can laboratories do?
To mitigate biotin interference, it is important for clinicians to be aware of patients’ biotin dosage regimen and renal function. These crucial details will have the greatest impact on reducing interference by determining instruction on dose withholding. The washout period varies for patients, but 8 hours is recommended for dosage of 5-10 mg daily whereas >= 72 hours is needed in patients on mega dose therapy of >= 100mg daily. Patients with renal insufficiency would require an even longer wash-out period.
If withholding supplementation is not feasible, then timing of the draw is the next most important step to mitigate interference. As an example, a patient who routinely supplements in the morning should be directed to delay their dose until after a morning blood draw, providing 24 hours between daily doses.
Other approaches to overcome biotin interference include:
- Re-analyze the sample with a different method
- Dilute the sample with dedicated assay diluent
- Remove excess biotin by use of streptavidin coated beads
Labs could consider repeat testing if biotin interference is suspected. However, this may be impractical depending on the patient’s transportation mode or physical and mental status. Thankfully, in some situations, assays most affected by biotin interference are also those that require serial measurements such as troponin. In these instances, true elevations could be detected upon serial measurements, helping to overcome the effects of biotin interference.
The bottom line, as noted by the FDA, is that lab personnel and developers and health care providers should be aware that biotin, which is often found in dietary supplements, can significantly interfere with some specific lab tests and, more importantly, cause incorrect test results. These incorrect results may go undetected1.
Notable is that since the time of the FDA notice related to biotin interference to the present day, many vendors have made significant improvements to assay performance, reducing biotin interference risks. Labs should first review manufacturer inserts for any new updates on the thresholds for biotin interference.
Overcoming Biotin Interference: The Long View
Biotin as an interfering factor can be minimized or eliminated by standardizing the preanalytical process as much as possible. Standardization of blood draws should include timing of sampling, diet, activities before sampling, body position, and preferably documentation of these variables as part of the test report. To mitigate biotin, labs should strive for controlling many of these same variables.
Understanding these factors and implementing appropriate measures to mitigate their effects is essential for ensuring high-quality laboratory testing and accurate clinical decision-making. For ultimate success, clinicians and laboratory personnel must work together to identify and address these preanalytical challenges, ultimately improving patient care and outcomes.
ABOUT THE AUTHOR
Tyler Radke, MLS(ASCP)CM is from Green Bay, WI, and graduated from the University of Wisconsin-Oshkosh. He is an ASCP certified medical laboratory scientist and the director of Laboratory & Pathology at Emplify Health. Radke has been at Emplify Health since 2015, providing comprehensive oversight of multiple high and moderate complexity laboratories. He is a member of the laboratory technical advisory group (LabTAG) for the Wisconsin Clinical Laboratories Network (WCLN). He is a regular contributor to CLP.
Reference
- “Biotin Interference with Troponin Lab Tests – Assays Subject to Biotin Interference.” U.S. Food and Drug Administration (FDA). June 21, 2022. https://www.fda.gov/medical-devices/in-vitro-diagnostics/biotin-interference-troponin-lab-tests-assays-subject-biotin-interference
Featured Image: Ekaterina79 | Dreamstime.com