Summary:
Rutgers and Yale engineers have developed a portable device that rapidly detects rare genetic mutations from a single drop of blood, aiming to bring PCR-level accuracy to point-of-care settings.
Takeaways:
- The device combines allele-specific PCR with electrical impedance on a microfluidic chip to detect mutations in under 10 minutes.
- It was successfully tested on six patient samples to detect hereditary transthyretin amyloidosis, a condition linked to heart failure.
- The researchers aim to integrate all testing steps into the chip and expand its ability to screen for multiple mutations simultaneously.
A team led by Rutgers University-New Brunswick engineers has developed a portable device capable of detecting rare genetic mutations from a single drop of blood.
The instrument, described in a study published in Communications Engineering of the Nature Publishing Group, was shown in lab experiments to quickly and accurately test for a genetic condition called hereditary transthyretin amyloidosis, which can cause heart problems.
The disease is caused by a genetic mutation in the transthyretin gene. This mutation can lead to heart failure, especially in people of West African ancestry. Detecting this mutation early is important because there are treatments available.
“Traditional genetic tests can take days or weeks to give results, which isn’t ideal for quick diagnosis,” says Mehdi Javanmard, PhD, a professor and Paul S. & Mary W. Monroe Endowed Faculty Scholar with the Department of Electrical and Computer Engineering in the Rutgers School of Engineering. “This research aims to develop a faster, cheaper and easier test that can be done during a regular doctor’s visit.”
Device Amplifies Nucleic Acid Segments
The device, which amplifies nucleic acid segments and detects mutations using a microchip, was developed in collaboration with Curt Scharfe and his team at Yale University. This new technology aims to bring a device equal to the performance and accuracy of a polymerase chain reaction (PCR) test, typically confined to laboratories, into doctors’ offices, homes and community centers.
The device resembles a PCR test but is more portable and quicker, yielding results within 10 minutes, according to the researchers, adding that the technology aims for rapid, point-of-care mutation detection.
“What we’ve figured out is how to make a device that has the potential to bring a kind of PCR testing, particularly in the context of detecting rare mutations, home, like a glucometer,” says Javanmard, an author of the study. “Imagine community centers having this. People with lower incomes don’t necessarily have ready access to such advanced testing techniques.”
The polymerase chain reaction is a lab technique used to amplify copies of specific segments of DNA. It is often used to detect the presence of pathogens such as viruses or bacteria or to help identify DNA from crime scene evidence.
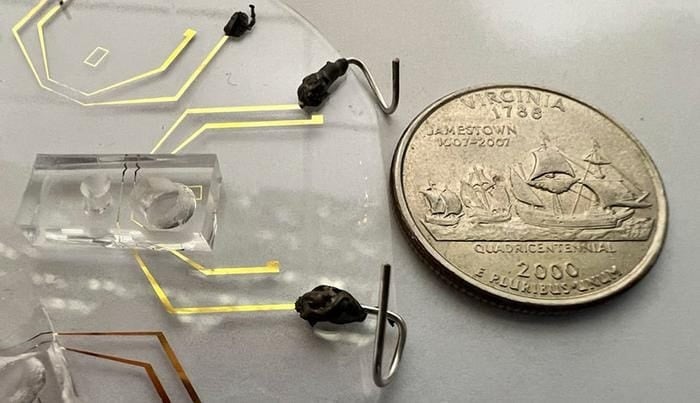
The new test combines a technique called allele-specific polymerase chain reaction, also known as ASPCR, with electrical impedance, which measures how the DNA samples affect the flow of electricity in microfluidic chips. These tiny chips, which can handle small amounts of liquid and measure electrical charges, differentiate DNA sequences from blood samples.
While PCR is a generalized technique used to amplify DNA segments, ASPCR is a specialized form of PCR used to detect mutations in DNA.
Genetic Mutation Testing Device Tested on Six Samples
The researchers tested their method on samples from six patients and accurately identified whether the patients had the mutation.
Researchers are working on improving the sensitivity and specificity of the technique as well as expanding its capabilities to detect multiple mutations simultaneously. This could lead to the development of comprehensive diagnostic tools that can screen for a wide range of diseases using a single test.
“The Holy Grail would really be to build a test that can do the top 20 different point mutations,” Javanmard says.
A point mutation is a change within a gene in which one base pair in the DNA sequence is altered. Such mutations are responsible for or contribute to many diseases, including sickle cell anemia, hemophilia and some cancers.
The researchers said they are confident because of the versatility of ASPCR, which can be tailored to detect many specific genetic mutations tied to diseases. In addition, microfluidic chips can be designed to detect different types of DNA or RNA sequences, giving them great potential for detecting various diseases.
“This technique holds great promise for detecting a variety of diseases, thanks to its versatility, speed and potential for cost-effective and portable diagnostics,” Javanmard says.
The technology is ready to be developed. Presently the ASPCR analysis, which can be used to make many copies of a DNA mutation directly from a tiny blood sample, is still being conducted outside of the microfluidic microchip. After this step, the results – the amplified DNA – can be detected by the microchip. Ultimately, the goal is to combine both processes, the ASPCR and the electric detection, directly on the microchip.
Other scientists who contributed to the study include Neeru Gandotra of Yale University, and Muhammad Tayyab and Jianye Sui in the Department of Electrical and Computer Engineering in the Rutgers School of Engineering.
Featured Image: A microfluidic device barely larger than a U.S. quarter and developed by a Rutgers University-led team can detect rare genetic mutations from a single drop of blood. Image: Rutgers University