By Abby Brody
Summary:
Despite powerful advances in precision medicine, most doctors remain untrained in these tools, leaving a critical gap between what science can do and what patients actually receive.
Takeaways:
- Traditional diagnostics are outdated and often detect disease only after significant damage has occurred, while newer tools can spot illness at the molecular level far earlier.
- Precision medicine technologies—like liquid biopsies, AI-enhanced imaging, and genomic profiling—are already improving outcomes in cancer, rare diseases, and even routine care.
- The main barrier is medical education, which hasn’t kept pace with scientific advancements; the American Board of Precision Medicine aims to close this gap by training physicians in these transformative tools.
For more than a century, the tools we use to peer inside the human body have remained almost frozen in time. The x-ray dates back to the nineteenth century. The stethoscope, the biopsy needle, the trusty blood-pressure cuff—all inventions of a pre-digital world. Even the once-dazzling CT scan and MRI, children of the late twentieth century, feel totally middle-aged today.
What began as miracles now look more like blunt instruments. They reveal damage only after it has taken hold, offering flat snapshots of biology that is anything but static. Worse, many of these staples expose patients to radiation that can sow the seeds of tomorrow’s cancers.
The Benefits of Precision Medicine
And yet, while traditional diagnostics have grown stale, biomedical science has raced ahead. Breakthrough tools that once lived exclusively in research basements and boutique clinics are spilling into everyday practice, promising to save lives long before patients sense that anything is amiss. The irony is cruel: the technology is ready, but most physicians have never been trained to wield it.
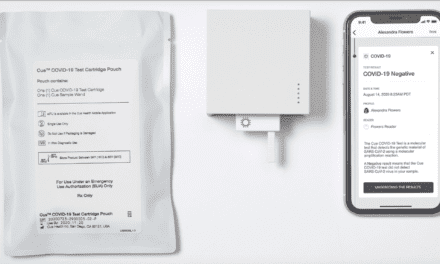
Consider what is already within reach. A single tube of blood can now be scoured for drifting fragments of tumor DNA, revealing a hidden cancer before the first shadow appears on a scan. Liquid biopsies offer a living window into the body after treatment, allowing oncologists to pounce on the faintest trace of residual disease instead of waiting months for a follow-up image. Artificial-intelligence engines sharpen every CT, MRI, and ultrasound, teasing out patterns that no human eye could hope to spot, sometimes years before symptoms would otherwise erupt. Outside oncology, microbiome and metabolomic analyses are exposing the earliest molecular tremors of autoimmune disorders and neurodegenerative decline, while wearable biosensors quietly stream heart rhythms and metabolic clues that once vanished between office visits.
We already know that precision works—when we choose to use it. In breast cancer, genomic profiling now spares nearly half of low-risk patients from the misery of chemotherapy without denting survival rates1. In pediatric leukemia, RNA sequencing has rescued countless children from overtreatment by unmasking mutations that older tests overlooked2. In neonatal intensive-care units, ultra-rapid genome sequencing can deliver a life-altering diagnosis in less than two days, an eternity shaved down to the blink of an eye when a newborn teeters between life and death3. Even in the humdrum world of primary care, population screening for familial hypercholesterolemia can catch a silent genetic killer early enough that a simple statin prescription prevents the heart attack that might have come out of nowhere4.
So why doesn’t every patient benefit? Because medical education still treats precision medicine as an elective curiosity. Most of today’s practicing physicians learned to manage the “average” patient with population-based algorithms, and the curriculum that forged them has barely kept pace with the science that now surrounds it. The chasm between possibility and practice is no longer an inconvenience; it is a public-health crisis.
Creating a Diagnostic Revolution
That crisis is why the American Board of Precision Medicine was born. I’m proud to be a founder and director of Patient Advocacy. Our mission is to prepare a new generation of clinicians who think in pathways and omics, who can read a genomic report as fluently as a chest x-ray, who understand that treating symptoms without tracing them to their molecular root is simply not good enough. By training doctors on the modern tools of today we can weave genomics, bioinformatics, and artificial intelligence into the very fabric of medical care.
As Anil Banjanth, MD, physician and founder of the AOPD asserts: “Precision medicine has fundamentally transformed the way I practice. It’s no longer about treating symptoms in isolation—it’s about connecting the molecular dots, peeling back the layers of complexity, and understanding that every patient’s pathophenotype has a different flavor. This approach allows me to move from generic protocols to deeply personalized interventions rooted in data, biology, and lived experience.”
We have spent a century diagnosing disease with yesterday’s tools. That era is over. From this point forward, the measure of medicine will not be how heroically we respond once illness strikes, but how early—and how precisely—we keep it from gaining ground at all. The diagnostic revolution has arrived. The science is mature, the infrastructure is standing, and the only missing ingredient is a physician workforce ready to wield the power now resting in its hands. If you believe health care must evolve, join us.
Help turn precision medicine from the exception into the rule. And now, thanks to the AOPM we will have doctors properly trained to leverage these advanced tools to create a revolution in healthcare.
ABOUT THE AUTHOR

Abby Levin Brody, M.S., is an educator, writer, speaker, founder and serves as director of Patient Advocacy at the American Board of Precision Medicine. Learn more at www.abbybrody.com and www.abopm.com.
References
- Cardoso, F., et al. (2016). New England Journal of Medicine.
- Ramaswami, G., et al. (2018). PMC6164147.
- Mauger, C., et al. (2022). Wired.
- Abul-Husn, N. S., et al. (2022). “Study on genomic screening for familial hypercholesterolemia.” PMC9584046.