Summary: A new study reveals that the nasal microbiota of ICU patients is more effective than gut microbiota in distinguishing sepsis from non-sepsis, providing new insights for diagnostic strategies.
Takeaways:
- Nasal microbiota analysis outperforms gut microbiota in predicting sepsis in ICU patients.
- Septic patients show significantly lower nasal microbiota community richness and distinct compositions.
- Key nasal bacteria like Corynebacterium, Staphylococcus, Acinetobacter, and Pseudomonas are enriched in septic patients, suggesting new biomarkers for sepsis diagnosis.
The nasal microbiota of intensive care unit (ICU) patients effectively distinguishes sepsis from non-septic cases and outperforms analyzing the gut microbiota to predict sepsis, according to a new study published in Microbiology Spectrum, a journal of the American Society for Microbiology.
“These findings have implications for the development of diagnostic strategies and advancements in critical care medicine,” says corresponding study author Xiaolong He, MD, PhD, a professor at the Microbiome Medicine Center, Department of Laboratory Medicine, Zhujiang Hospital, Southern Medical University, Guangzhou, Guangdong, China. “In the past, we have paid more attention to the intestinal microbiota of sepsis patients, and the respiratory microbiota also deserves our attention.”
The Impact of Sepsis
Sepsis is a severe illness with a high mortality rate between 29.9% to 57.5%. Despite the establishment of the third international consensus definition of sepsis and septic shock (Sepsis-3) in 2016, there are still many aspects of sepsis that warrant further exploration to improve its diagnosis. The evolution of the diagnostic criteria from Sepsis-1 to Sepsis-3 shows the need for continued investigation. Additionally, sepsis diagnostic criteria have shifted from focusing solely on the inflammatory response to also including organ failure caused by infection. While considerable progress has been made in the diagnosis of sepsis, no biological indicators with strong sensitivity and specificity have been identified. Furthermore, the low culture positivity rate and the presence of few culturable microorganisms limit the diagnosis of clinical sepsis. Therefore, the identification of a new, effective and reliable biomarker for sepsis has been a goal of researchers.
Further reading: New Sepsis Test Provides Faster and Reliable Results
New Sepsis Study
In the new study, researchers recruited 157 subjects (89 with sepsis) of both sexes at the affiliated hospital of Southern Medical University. They collected nasal swabs and fecal specimens from septic and non-septic patients in the ICU and Department of Respiratory and Critical Care Medicine. The scientists extracted and sequenced DNA using Illumina technology. Bioinformatics analysis, statistical processing, and machine learning techniques were used to differentiate between septic and non-septic patients.
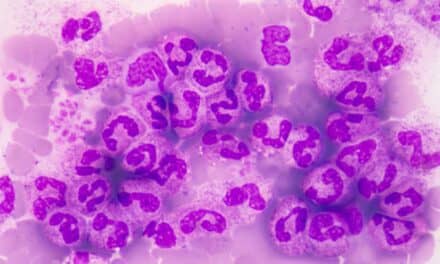
He and colleagues discovered that nasal microbiota of septic patients exhibited significantly lower community richness (P=0.002) and distinct compositions (P=0.001) compared to non-septic patients. Corynebacterium, Staphylococcus, Acinetobacter and Pseudomonas were identified as enriched genera in the nasal microbiota of septic patients.
“Looking forward, we suggest the potential for further research, possibly through animal models or larger patient cohorts, to deepen our understanding of microbiota’s role in sepsis beyond the antibiotic effect,” he says.