Improving outcomes with sepsis is dependent on timely diagnosis and treatment. While blood-culture-based tests are the gold standard, culture-independent testing can shave off critical days between diagnosis and treatment.
By Aparna Ahuja, MD, and Devon McCleary, PharmD
Bloodstream infections (BSIs), such as bacteremia and fungemia, cause increased incidences of morbidity and mortality. If left untreated, BSIs can quickly progress to sepsis, an inflammatory response to an infection that can result in organ system failure and death.1,2 As a burdensome condition worldwide, sepsis accounts for almost 49 million cases and 20% of deaths annually.3 Patient outcomes are significantly influenced by the time to diagnosis and initiation of targeted treatment. In the United States alone, the Centers for Medicare & Medicaid Services (CMS) estimates that sepsis contributes to more than $62 billion annual spending in admissions for both inpatient and skilled nursing facilities.4
Timely Diagnosis of BSIs
It is recommended to immediately start prophylactic treatment in patients who are at a high likelihood for sepsis and suspected of BSI.5 Treatment is often started prior to confirming diagnosis of BSI and with broad-spectrum antimicrobial therapy. Broad-spectrum therapies are often considered first-line treatments due to their broad coverage of targeting various pathogens, even though they do not necessarily target the individual patient’s specific disease.
Blood cultures are recognized as the gold standard for diagnosing BSIs as they detect whether there is an infection in the blood. If positive, additional follow-up techniques are necessary to identify which species of pathogens are causing the infection in the patient.
Blood cultures are the primary diagnostic tests for BSI, although there are some disadvantages. For example, blood culture-based species identification may take a few days to achieve microbial growth. This may delay altering treatment from broad-spectrum therapy to appropriate targeted therapy, which could lead to a poor outcome for a patient who has a serious BSI. In addition, antimicrobial administration prior to blood collection and incorrect sample collection techniques may also result in negative culture results.6,7 It has been acknowledged that blood culture may miss approximately 50% of episodes of invasive candidiasis as blood cultures are limited due to their poor sensitivity, slow time to growth, and slow species identification.8 While blood culture is an important tool in diagnosing and preventing sepsis, patients could benefit from tests that provide faster and more accurate results.
Multiple diagnostic tests have been developed to assist with the diagnosis of BSIs. The information gathered from these testing techniques allows clinicians to appropriately diagnose and treat infectious bloodborne illnesses with antimicrobials that are specified for the organisms detected.
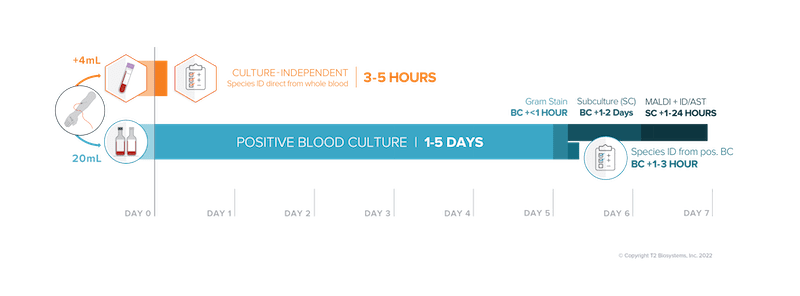
There are many factors involved in reviewing diagnostic tests, one of the most important being time to result. The traditional workflow that follows a positive blood culture includes a gram stain to confirm the presence of bacteria or fungi. Next, various techniques that rely on a positive blood culture can be used to identify the species. Amplification of DNA sequences using polymerase chain reaction (PCR) targets certain predetermined pathogens for identification. Matrix-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOF) relies on bacterial enrichment and purification from a positive blood culture for microbial classification and diagnosis. In situ hybridization tests detect microorganisms in samples using nucleic acid mimics. Metagenomic shotgun sequencing uses a wide variety of nucleic acids to identify pathogens.9
Culture-independent diagnostic tests that utilize magnetic resonance are not reliant on the blood cultures turning positive for species identification. Magnetic resonance utilizes cell lysis, PCR, and superparamagnetic nanoparticles within a magnetic field to provide species-level identification. Because of this, culture-independent tests can deliver more timely results compared to molecular tests that are dependent on the results of blood cultures.9
A Growing Problem with Treating Sepsis
The prolonged administration of broad-spectrum antibiotic therapy and overprescribing inappropriate therapies are associated with antimicrobial resistance (AMR). AMR occurs when infections are no longer responsive to medicines thus becoming more difficult to treat. Several bacterial and fungal pathogens have been recognized by the Centers for Diseases Control and Prevention (CDC) as antimicrobial resistance threats in the United States.10 Globally, the World Health Organization (WHO) has identified AMR as one of the top 10 public health threats leading to treatment complications and increased mortality and a recent study showed that AMR was the leading global health issue in 2019.11, 12 Despite advances in medicine, the world continues to struggle with AMR as a dangerous consequence to the overuse and inappropriate use of antimicrobials. Controlling AMR through early diagnosis of BSIs and timely targeted therapy may be a practical solution for prevention.
Time is an important factor in the prevention of AMR and sepsis. Early identification and treatment of sepsis is essential; for every hour of delay in appropriate therapy, survival decreases by almost 8%.13 One clinical trial observed inappropriate antimicrobial use in 37.2% of patients, which could be improved with better and timely diagnostic testing.14 With faster diagnosis, clinicians can initiate de-escalation of antimicrobial therapy to a targeted and effective agent as soon as a pathogen is identified. De-escalation of antimicrobial therapy is associated with less antimicrobial resistance, fewer side effects, and lower healthcare costs.15 The application of new molecular techniques in microbiological diagnosis enables faster identification of causative pathogens. Other positive outcomes such as reduction in length of hospital or intensive care unit (ICU) stay and reduction in organ injury can be achieved with faster and accurate diagnosis.16-19
When treating suspected BSIs, there are several bacterial and fungal species that are of concern due to the incidence and severity of the infections. The ESKAPE (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species) pathogens are a group of infectious bacteria that have garnered particular attention for their ability to escape or evade common therapies through antimicrobial resistance.20 For fungal infections, Candida species are of interest due to the high risk of drug resistance which is recognized as a serious threat to AMR by the CDC.21 There are many Candida species that have been identified to cause infections in humans, however, >90% of invasive candidiasis are caused by the following five Candida species: C. albicans, C. tropicalis, C. parapsilosis, C. glabrata and C. krusei.22 Because of the importance of early diagnosis of these pathogens, tests that address these pathogens in a timely manner are beneficial to sepsis diagnosis and management.
Using Novel Technology to Improve Timely Diagnosis of BSI
Ideally, diagnostic testing would have a fast turnaround time with low limit of detection to allow doctors to prescribe patients with appropriate antimicrobial therapy faster. Culture-independent molecular diagnostic tests can have an impact on antimicrobial stewardship programs and improve quality of care in patients with sepsis. The principles of antimicrobial stewardship include using appropriate targeted therapy and limiting inappropriate use of therapies.23 Early diagnostic tests are essential tools in antimicrobial stewardship programs for healthcare providers to make quick, accurate, and informed decisions regarding patients’ treatment. Better diagnostic options ultimately have the potential to increase quality of life and survival outcomes in vulnerable patients at risk of developing BSIs with highly resistant organisms.
Culture-independent molecular diagnostic tests such as the T2Bacteria and T2Candida Panels are FDA-cleared and CE-marked tests utilizing the T2MR Technology platform to identify bacteremia and candidemia, respectively, directly from a whole blood sample in 3 to 5 hours, while simplifying the collection process by eliminating the need for sample preparation.24-25
Studies for T2MR Technology have shown a significant reduction in time to detection/species identification, a potential reduction in length of ICU and overall hospital stays, a likely decrease in cost per patient, faster de-escalation of broad spectrum medications, and the opportunity for a targeted approach in antimicrobial therapy for better patient outcomes when compared to blood culture.26,27 Usage of these culture-independent tests in the right patient population can improve clinical and healthcare outcomes by detecting many of the problematic sepsis-causing ESKAPE and Candida species pathogens sooner, resulting in earlier administration of appropriate targeted antimicrobial therapy.
Enhancing Patient Care with Diagnostic Advancements
Rapid and effective antimicrobial therapy is crucial to improve septic patient outcomes, while inappropriate empirical therapy is a well-known, strong, independent predictor of mortality. Multidrug-resistant organisms have escalated to a pandemic level during the last two decades. Early identification of pathogens that are known to be multi-drug resistant has the potential to positively affect sepsis management and reduce antimicrobial resistance by targeting therapy sooner.
(Editor’s note: an earlier version of this article listed the incorrect author. It has been corrected with the authors’ names by CLP staff.)
About the Authors
Aparna Ahuja, MD, is the former chief medical officer at T2 Biosystems, providing leadership and strategic direction for medical, clinical, scientific, and regulatory activities. Ahuja possesses extensive global experience in laboratory medicine and medical device-in vitro diagnostics. Most recently, she served as worldwide vice president, Medical Affairs at Becton Dickinson, where she was responsible for global medical leadership, setting and leading the strategy for medical affairs, clinical development, and key opinion leader engagement in support of new product development, lifecycle management, and compliance. Prior to Becton Dickinson, Ahuja held a variety of roles in clinical practice, research, academia and IVD, where she has been focused on continuous improvement and innovation in diagnostics, stressing precision, and rapid turnaround times. A certified auditor with ISO 15189 & College of American Pathologists, Ahuja has successfully led and guided pathology laboratories through audits and inspections from CAP, ISO 15189, ANVISA, CDC, and the FDA. She is an active member of the American Association of Clinical Chemistry (AACC), College of American Pathologists (CAP), American Society of Microbiology (ASM), Clinical and Laboratory Standards Institute (CLSI), European Federation of Clinical Chemistry and Laboratory Medicine (EFLM), and serves as Chair of AACC New Jersey section, vice-chair of CLSI’s Expert Panel, chair of the Corporate Advisory Board AACC, and Scientific Advisory Board member of PainCare Labs. As an ardent speaker, she presents at international laboratory medicine conferences and has many peer-reviewed publications to her credit.
Devon McCleary, PharmD, is a pharmacist and former medical information specialist at T2 Biosystems. McCleary’s career has focused on providing individualized care to patients and accurate information to aid in the clinical decision-making process for medical professionals. Her position supports the Medical Affairs team through research, writing, and collaboration with field specialists to provide evidence-based and nonpromotional information regarding diagnostic devices.
References
1. Buehler SS, Madison B, Snyder SR, et al. Effectiveness of practices to increase timeliness of providing targeted therapy for inpatients with bloodstream infections: a laboratory medicine best practices systematic review and meta-analysis. Clin Microbiol Rev. 2016;29(1):59-103.
2. Seymour CW, Liu VX, Iwashyna TJ, et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):762-74.
3. Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study. Lancet. 2020 Jan 18;395(10219):200-211.
4. Buchman TG, Simpson SQ, Sciarretta KL, et al. Sepsis among Medicare beneficiaries: 3. the methods, models, and forecasts of sepsis, 2012–2018. Crit Care Med. 2020;48(3):302-318.
5. Evans L, Rhodes A, Alhazzani W, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021. Crit Care Med. 2021 Nov 1;49(11):e1063-e1143.
6. Cheng MP, Stenstrom R, Paquette K, et al. Blood Culture Results Before and After Antimicrobial Administration in Patients with Severe Manifestations of Sepsis: A Diagnostic Study. Ann Intern Med. 2019 Oct 15;171(8):547-554.
7. Scheer CS, Fuchs C, Gründling M, et al. Impact of antibiotic administration on blood culture positivity at the beginning of sepsis: a prospective clinical cohort study. Clin Microbiol Infect. 2019 Mar;25(3):326-331.
8. Clancy CJ, Nguyen MH. Finding the “missing 50%” of invasive candidiasis: how nonculture diagnostics will improve understanding of disease spectrum and transform patient care. Clin Infect Dis 2013;56:1284-1292.
9. Eubank TA, Long SW, Perez KK. Role of Rapid Diagnostics in Diagnosis and Management of Patients With Sepsis. J Infect Dis. 2020 Jul 21;222(Suppl 2):S103-S109.
10. Centers for Disease Control and Prevention. Drug-Resistant Candida Species. https://www.cdc.gov/drugresistance/biggest-threats.html. Published 2021. Accessed January 12, 2021.
11. World Health Organization. Antimicrobial resistance. https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance#:~:text=Antimicrobial%20resistance%20%28AMR%29%20is%20a%20global%20health%20and,top%2010%20global%20public%20health%20threats%20facing%20humanity. Accessed January 12, 2021.
12. Murray, C. J., Ikuta, K. S., Sharara, F., Swetschinski, L., Aguilar, G. R., Gray, A., … & Naghavi, M. (2022). Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet.
13. Kumar A, Roberts D, Wood KE, et al: Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006; 34:1589–1596.
14. Fridkin SK, Baggs J, Fagan R, et al. Vital signs: improving antibiotic use among hospitalized patients. MMWR Morb Mortal Wkly Rep. 2014;63(9):194-200.
15. Pollack LA, van Santen KL, Weiner LM, et al. Antibiotic stewardship programs in U.S. acute care hospitals: findings from the 2014 National Healthcare Safety Network Annual Hospital Survey. Clin Infect Dis. 2016;63(4):443–449.
16. Zhang D, Micek ST, Kollef MH. Time to appropriate antibiotic therapy is an independent determinant of postinfection ICU and hospital lengths of stay in patients with sepsis. Crit Care Med. 2015;43:2133–2140.
17. Bagshaw SM, Lapinsky S, Dial S, et al; Cooperative Antimicrobial Therapy of Septic Shock (CATSS) Database Research Group: Acute kidney injury in septic shock: clinical outcomes and impact of duration of hypotension prior to initiation of antimicrobial therapy. Intensive Care Med. 2009; 35:871–881.
18. Iscimen R, Cartin-Ceba R, Yilmaz M, et al: Risk factors for the development of acute lung injury in patients with septic shock: an observational cohort study. Crit Care Med. 2008; 36:1518–1522.
19. Centers for Disease Control and Prevention. The Core Elements of Hospital Antibiotic Stewardship Programs: 2019. https://www.cdc.gov/antibiotic-use/healthcare/pdfs/hospital-core-elements-H.pdf. Published 2019. Accessed September 13, 2021.
20. Boucher HW, Talbot GH, Bradley JS, et al. Bad bugs, no drugs: no ESKAPE! An update from the Infectious Diseases Society of America. Clin Infect Dis. 2009;48(1):1-12.
21. Centers for Disease Control and Prevention. Drug-Resistant Candida Species. https://www.cdc.gov/drugresistance/pdf/threats-report/candida-508.pdf. Published 2019. Accessed September 13, 2021.
22. Pappas PG, Kauffman CA, Andes DR, et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62:e1-50.
23. Garnacho-Montero J, Aldabo-Pallas T, Garnacho-Montero C, et al: Timing of adequate antibiotic therapy is a greater determinant of outcome than are TNF and IL-10 polymorphisms in patients with sepsis. Crit Care. 2006; 10:R111.
24. Mylonakis E, Clancy CJ, Ostrosky-Zeichner L, et al. T2 magnetic resonance assay for the rapid diagnosis of candidemia in whole blood: a clinical trial. Clin Infect Dis 2015;60:892-829.
25. Nguyen MH, Clancy CJ, Pasculle AW, et al. Performance of the T2Bacteria Panel for Diagnosing Bloodstream Infections: A Diagnostic Accuracy Study. Ann Intern Med. 2019;170(12):845-852.
26. Giannella M, Pankey GA, Pascale R, et al. Antimicrobial and resource utilization with T2 magnetic resonance for rapid diagnosis of bloodstream infections: systematic review with meta-analysis of controlled studies. Expert Rev Med Devices. 2021;18(5):473-482.
27. Kenney R, Dwivedi S, Kendall R, et al. Implementation of T2 magnetic resonance into the antimicrobials stewardship program improves management of candidemia at HFHS. Poster presented at: ID Week; October 2016; New Orleans, LA.





