Washington University researchers are developing a rapid test to classify sepsis patients into inflammatory profiles for targeted treatment.
Researchers at Washington University School of Medicine in St. Louis received a $4.87 million grant from the US Department of Defense to develop a handheld diagnostic device that can rapidly classify sepsis patients into distinct inflammatory profiles.
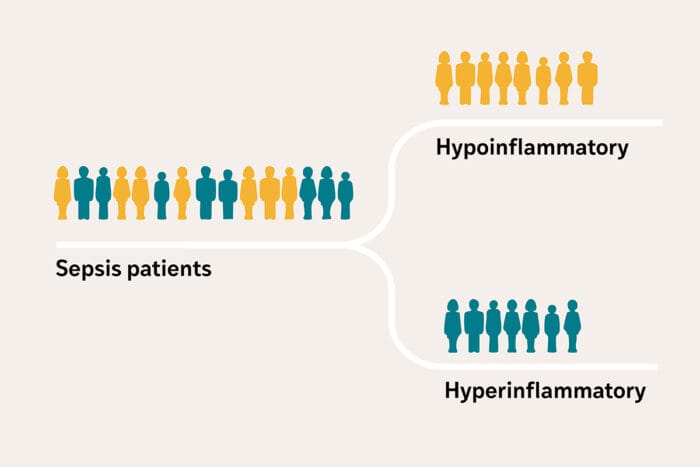
The device will measure two biomarkers—interleukin-8 (IL-8) and soluble tumor necrosis factor receptor 1 (sTNFR-1)—to categorize patients with sepsis into either a high-risk hyperinflammatory profile or a less severe hypoinflammatory profile. This classification could enable targeted treatments that address the variability in biological responses among sepsis patients with similar symptoms.
“Developing a precise test and an affordable device to quickly identify patients with the high-risk hyperinflammatory profile is crucial for delivering targeted treatments and saving lives in critical situations when time matters,” says Pratik Sinha, MBChB, PhD, assistant professor in the Department of Anesthesiology at WashU Medicine and lead researcher on the project, in a release. “A highly portable device will enable deployment in active military and combat zones, where trauma increases the risk of infection and sepsis.”
Addressing Treatment Variability
Sepsis affects at least 1.7 million people annually in the US, with a mortality rate of roughly 21%. The mortality rate increases to around 50% in patients with the hyperinflammatory profile. Current treatments include antibiotics and supportive therapy for damaged organs, but this approach does not address the body’s dysregulated response to infection.
“Current treatments don’t address the body’s dysregulated response to the infection,” says Sinha in a release. “The challenge in delivering effective treatments is the variability in the severity of the biological response among patients with similar symptoms.”
An earlier study of 3,000 people with critical illness by Sinha and colleagues, published in The Lancet Respiratory Medicine, found that blood levels of IL-8 and sTNFR-1 were reliable indicators of whether a person has a high or low inflammatory response. When researchers performed secondary analysis using data from two previously conducted clinical trials and categorized patients into the two inflammatory profiles, they found that treatment efficacy differed between the two groups.
Lateral Flow Technology with Enhanced Sensitivity
The research team is collaborating with Srikanth Singamaneni, PhD, the Lilyan & E Lisle Hughes Professor at the McKelvey School of Engineering at WashU, to develop a lateral flow test similar to a COVID-19 rapid antigen test. Unlike standard rapid tests that only indicate presence or absence of a target, this test incorporates plasmonic fluors—small particles that glow—to measure the amount of each inflammatory protein captured on the strip.
“The biomarkers we are trying to detect are found in very small concentrations in the blood,” says Singamaneni, who developed the lateral flow system that incorporates the plasmonic fluors, in a release. “Incorporating the fluorescent nanoparticles into the test renders it extremely sensitive, allowing us to not only detect but also accurately measure these biomarkers.”
The plasmonic fluor technology has been patented and licensed to Brightest Bio, a WashU startup formerly called Auragent BioSciences, by WashU’s Office of Technology Management.
Portable Design for Multiple Settings
The researchers are developing the test and device to be affordable, accurate, and fast. The device will include a camera to detect the glowing particles and a computer model to quantify the levels for patient categorization. Its compact and portable design will allow deployment in various critical care settings, including military bases, combat zones, and rural hospitals.
“This tool has the potential to reach patients at the bedside, offering personalized care based on each individual’s specific biological responses,” says Sinha in a release. “We hope to fill a need in critical care that will help bring more effective treatments to more patients.”
The grant was awarded through the Peer-Reviewed Medical Research Program under Award Number HT9425-25-1-0825, supported by the Assistant Secretary of Defense for Health Affairs.
Photo caption: Researchers are developing a rapid test to classify sepsis patients into inflammatory profiles for targeted treatment.
Photo credit: Sara Moser