High-grade serous carcinoma identified in cervical biopsies is overwhelmingly secondary to upper genital tract tumors, most commonly of endometrial origin, the study finds.
A new clinicopathologic study provides evidence supporting the World Health Organization’s (WHO) decision to exclude cervical serous carcinoma from its 2020 classification, finding that nearly all high-grade serous carcinomas identified in cervical biopsies actually originate from other sites in the reproductive tract.
The retrospective study, published in the Journal of Clinical and Translational Pathology, analyzed 59 cases originally diagnosed as “serous carcinoma” or “high-grade serous carcinoma” in cervical or endocervical biopsies collected between 2013 and 2023. Researchers found that 96% of these tumors originated from the endometrium (47 cases) or the tubo-ovarian region (4 cases), with only one case confirmed as a primary cervical carcinoma.
The findings have implications for clinical laboratories, as accurate tumor classification directly impacts patient management and treatment decisions. Misclassification of these tumors as primary cervical cancers could lead to inappropriate treatment protocols.
Diagnostic Challenges and Laboratory Implications
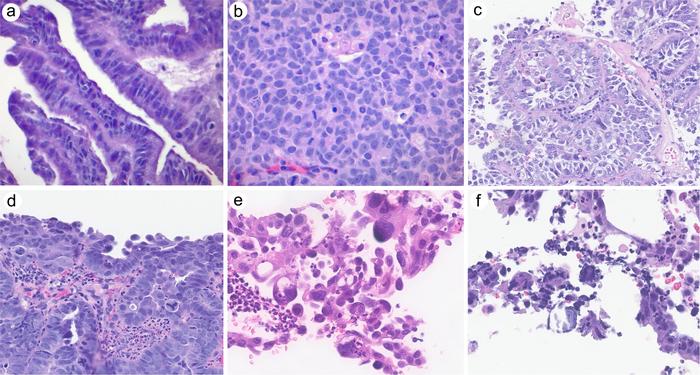
The study revealed that morphologic patterns in these tumors varied considerably and could mimic human papillomavirus-associated adenocarcinoma, presenting diagnostic challenges for pathologists. All tumors showed aberrant p53 expression and diffuse p16 positivity, markers that laboratories routinely use in cancer diagnosis.
However, the research identified key differentiating immunohistochemical profiles that can aid in accurate classification. WT-1 was expressed in all tubo-ovarian tumors but in only 12% of endometrial cases. Estrogen receptor and progesterone receptor were frequently positive in endometrial tumors, while human epidermal growth factor receptor 2 was positive in 31% of cases.
Molecular analysis performed on a subset of cases confirmed tumor protein p53 mutations and other alterations typical of uterine serous carcinoma, supporting the use of targeted next-generation sequencing in differential diagnosis.
Impact on Laboratory Practice
The study emphasizes the importance of comprehensive diagnostic workups when high-grade serous carcinoma is identified in cervical biopsies. Clinical laboratories should consider additional testing, including radiologic correlation and molecular profiling, to determine the true origin of these tumors.
The research also highlights that a small subset of endocervical adenocarcinomas may mimic serous carcinoma, requiring careful morphologic and immunohistochemical evaluation to avoid misclassification.
These findings support current WHO classification guidelines and reinforce the need for laboratories to maintain updated diagnostic criteria. The study suggests that when high-grade serous carcinoma is identified in cervical specimens, pathologists should strongly consider secondary involvement from upper genital tract primaries rather than assuming cervical origin.