Flow cytometry labs are under increasing pressure due to time, regulatory, and budgetary constraints. However, there are proven ways to streamline workflow efficiency to benefit both the lab’s bottom line and patient care.
By Lisa Holey, Dr.rer.nat
There are two main use cases for diagnostic flow cytometry: standardized IVD assays cleared or certified by regulatory agencies, and user laboratory-defined tests. The first uses systems and reagents manufactured by the IVD medical device industry for IVD purposes, based on the respective intended use of an assay, for example, to enumerate CD4+ T cells for HIV monitoring. Standardized assays are also used as a secondary metric for determining immune cell frequency in patients who have general changes in white blood cells of unknown origin.
The second application is more complex and makes use of tests developed by laboratories for diseases that have no clear-cut diagnostic guidance. These user-defined tests allow laboratories to customize assays based on their individual medical expertise and needs. Potential applications include, but are not limited to, monitoring patients after solid organ transplantation or those undergoing immunotherapy.
While flow cytometry offers labs a lot of flexibility to diagnose a variety of diseases, several aspects of these tests put a lot of strain on the labs performing them. The first is sample preparation and the manual handling involved in it. Diagnostic flow cytometry labs are subject to patient safety regulations and must achieve accuracy and precision to ensure quality results. However, flow cytometry is a time-consuming process that involves many steps, such as washing the sample, which can introduce variability and bias based on how they are performed. It can be hard to find technicians to run these assays, as it is difficult to train people to support these complex workflows. On top of that, most flow cytometry labs need to generate revenue or operate within a tight budget, with little room for error or repetitive testing. This leaves flow cytometry labs needing to do more with less.
Streamlining Flow Cytometry Lab Workflows
Luckily, there are ways for them to streamline their operations in order to achieve that feat. The first focuses on how flow cytometry labs design their panels and prepare their reagents. To take some of the burden out of reagent prep, dried-down reagent cocktails that are pre-prepared and tested are available for standardized assays. Reconstituting these cocktails is much faster than pipetting all of the antibodies in a panel, so the burden of reagent prep is reduced during manual processing.
In addition to panel design and preparing reagents, labs can optimize their inventory management in order to be more time- and cost-efficient. One way is to make standing orders for regular reagents needed for flow cytometry, such as positive and negative controls or sheath fluid. This reduces the need to monitor inventory, and decreases the chance of forgetting to order. Also, it can be helpful to designate a point person who manages inventory. In fact, many flow cytometry labs already do this. A point person can efficiently catalogue and store deliveries, and document things like shelf life and when reagents were opened. This can be important for streamlining inventory management and maintaining full compliance with audit requirements.
Labs can also tweak their workflow in order to streamline their flow cytometry operations. There are simple changes, such as being tidy and organized, having all reagents at hand, and designating workspace close to key instruments that can make manual processing more efficient. Another key way to improve efficiency is by batch processing. By batching samples, you can handle lots of similar samples at the same time and speed up processing. Unfortunately, the timing of samples arriving in the lab can make this unrealistic, and prolong time to result for the individual patient.
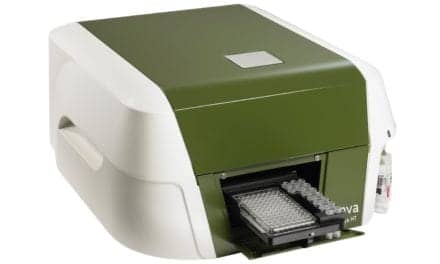
One potential solution that resolves many of the issues faced by flow cytometry labs is automation. Automating steps involved in sample processing can significantly reduce the manual parts of the workflow, help improve reproducibility and reduce errors, which leads to fewer repeat tests. While very few labs currently have full-process automation available to them, partial automation—through the use of a cell wash centrifuge or lysing station—is frequently used.
While automation represents a big step towards streamlining diagnostic flow cytometry, there are still areas that can be improved in the future to boost efficiency. The first major area is digitalization of data recording. Diagnostic labs must document many patient details, and this represents a high workload and a huge potential source of error. While solutions are available to support data reporting, many labs still report data manually, and could therefore benefit from automating data reporting.
One aspect of the diagnostic process that could be improved in the future is sample re-analysis and final diagnosis. Manually gating results can introduce bias, but incorporating artificial intelligence or diagnostic aids can make reanalysis simpler, and still let users have the final say in the decision-making process.
Flow cytometry is a flexible diagnostic tool that is used in many clinical contexts, and provides a framework for the detection of new markers as they arise. However, flow cytometry labs are under a lot of strain from technical, time, regulatory, and budgetary constraints. Fortunately, there are ways for labs to be more efficient in their panel design, reagent prep, inventory management, and sample processing, all of which can help them do more with less.
Streamlining is not something that only benefits a flow cytometry lab’s productivity or bottom line. Being more efficient can ease employee workloads and help improve their work-life balance.
About the Author
Lisa Holey, Dr.rer.nat, is a global strategic brand manager for clinical flow cytometry at Beckman Coulter Life Sciences. Based near Berlin, Germany, she supports strategic and commercial marketing activities to foster customer-centric workflow concepts with the aim to improve patient care. Her background and passion are in science. She started her career investigating the interplay of different immune cell subsets in the cancer microenvironment trying to identify new targets for immune modulating therapies.