HSV reagent
Serology is the scientific study of serum. In medicine, it refers to the diagnostic identification of antibodies in the serum obtained from a patient’s blood sample. In practice, it has many applications.
Lab Tests Online, a site produced by the American Association for Clinical Chemistry (AACC), cites six reasons to perform an antibody test (qualitative or quantitative): to document exposure to an infectious or foreign agent; to evaluate the protection level or immune status against a particular microorganism; to diagnose an autoimmune condition; to diagnose the reason for a transfusion reaction or the rejection of a transplanted organ; to diagnose an allergy; or to monitor the course of an infection or autoimmune process.
“Since it is such a broad field, it means there are a great many technologies that are in use in serology testing,” says Henry Homburger, MD, laboratory director of the Immunology Reference Lab at Phadia AB in Portage, Mich, and professor emeritus at the Mayo Medical School in Rochester, Minn. These tests may be commercially available through a “great many manufacturers” or developed in-house, often at universities and tertiary care centers, according to Homburger.
With the large numbers of tests currently available (and in development), Homburger sees the main trend in serology as continuing growth, particularly in applications. “New technology allows us to better define the nature of the antigens. For example, recombinant technology allows us to combine certain antigens that in the past we couldn’t produce that way, so we have now large supplies of antigens that were previously quite rare,” Homburger says.
In addition, new technologies can also improve the performance of existing applications. “There is also a trend to switch some serology tests to molecular methods. Until recently, this was limited to specific tests—like Chlamydia testing, for example—but with automation and cost reduction of NAT [nucleic acid technology] testing, there is a trend to expand NAT to other pathogens,” says Ann Madden, clinical microbiology division manager for Bio-Rad Laboratories, Hercules, Calif.
Automation, a major trend in the clinical laboratory in general, is also a trend in serology. “Serology testing is moving from manual or semiautomated systems to fully automated platforms. This allows labs to consolidate their serology testing with other activities—chemistry, immunochemistry, etc—and to rationalize their workflow and suppliers,” Madden says. Automation can also enable better accuracy, shorter turnaround, less hands-on time, and greater cost efficiency.
Today’s Technologies

BioPlex 2200
Homburger sees three main methodologies in use for serology testing today: indirect immunofluorescent microscopy, or IFA, an older slide-based methodology, “where the antigens are contained in a substrate that sticks to the slide;” enzyme-linked immunoabsorbent assays, or ELISAs, during which “the antigens are adsorbed through the walls of microtiter plates”; and the newest, multiplex technology, “where the antigens are coupled covalently to polystyrene beads,” Homburger says.
The newer technologies offer improvements over older methods (as expected) but, still, are not perfect. “I think when we talk about serologies and the quest for the identification and quantitation of antibodies, I think every technology has its drawbacks,” says Dave Kolesar, ELISA marketing manager for Alere (formerly Inverness Medical) in Princeton, NJ.
IFA, for instance, suffers from its subjective nature and lack of instrument standardization, which becomes evident when comparing various microscopes and finding the results are not uniform. Kolesar offers the enormous range in accepted responses published by the College of American Pathologists (CAP) as evidence of this challenge, saying, “It’s a difficulty and clearly a weakness.”
ELISAs perform better but generally require laboratorian time and may require longer turnaround times. “However, their cost remains lower than molecular methods and their analytical performances are usually excellent,” Madden says.
Molecular methods perform even better. “NAT are perceived as the ‘gold standard’ methods due to high levels of specificity and sensitivity, but their cost is significantly higher,” Madden says. However, they also offer greater reproducibility, objectivity, and quick turnarounds.
“So the strengths of the newer technologies are speed, ease of performance in the laboratory, and lack of dependence on the expertise of the technologist to interpret results,” Homburger summarizes. Because of the expected stresses in the clinical laboratory (low staffing levels, high volumes, etc), manufacturers plan to continue to improve these parameters with greater automation, easier use (newer generations are rated moderate complexity), and more reproducibility.
Seeking Standardization
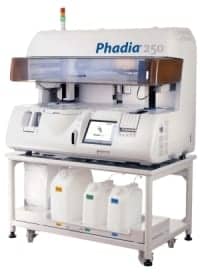
Phadia 250
Homburger, however, would also like to see greater standardization in the field as a whole. “The weaknesses of the newer technologies tend to be that they’re not necessarily well standardized one against the other. So, for example, the cutoffs for positives [for enzyme immunoassays] tend to vary from company to company,” Homburger says.
Many of the enzyme immunoassays may not carry the same antigens or combination of antigens. “This has become an issue with organizations like the American College of Rheumatology [ACR], where they have recommended that indirect immunofluorescent microscopy still be considered the gold standard for clinical applications because of the fact that, historically, all of the antigens are present in the substrate,” Homburger says.
Different ELISA tests can, therefore, produce different results. “You can get a weak positive or a positive response from one method and a negative response or quite a different response with another,” Homburger says. This, naturally, has implications for clinical use: Physicians tend to use the information in conjunction with other factors, such as the patient presentation and clinical impression.
For instance, new ACR guidelines for the determination of rheumatoid arthritis list the criteria to evaluate when deciding on a diagnosis; included in the assessment are three serology tests. “A score of six or more [out of 10] is required to make a presumptive diagnosis. So clearly serology plays a role, but it’s not the only role,” Kolesar says.
Understanding Variability
The patient’s demographics and sample characteristics will also play a role in the interpretation of laboratory results as well as the determination of a diagnosis and interpretation of results. In general, people do not produce antibodies at the same rate, which complicates matters. For instance, patients with compromised immune systems often have abnormal responses and may produce antibodies more slowly than a healthy human.
“Patient variability—age, sex, ethnic origin, clinical status, etc—is a real issue as it makes it hard to recruit sufficient numbers and volumes of samples that statistically represent the population targeted by the test,” Madden says. To develop such a panel takes more time and cost and, therefore, becomes an important factor for the manufacturer to consider during early development stages.
“I think the FDA has done a pretty good job in that respect with recommending that manufacturers run challenges for potentially interfering substances. So now, when you read a package insert, the performance section will tell you what patient factors potentially affect the results,” Kolesar says. Similarly, studies on the test’s reproducibility are also completed and included within the product information. “[Laboratorians] can find what tests were performed and what the variability inherent to that particular assay is likely to be,” Kolesar says.
However, if a physician doesn’t understand this information (or doesn’t look at it), the result interpretation may be compromised. “I don’t know that physicians across the board understand the relationship between patient variability and variability in test results,” Homburger says.
In addition, there is not always a precise relationship between a serologic test result and the patient’s clinical status (such as allergy, connective tissue disease, etc). “Somebody with rather profound symptoms might have rather low levels of antibodies and vice versa,” Homburger says.
The industry would, therefore, benefit from a database that is able to compare methods as well as capture clinically useful information about the tests themselves. “It would put the customer in a much more advantageous position in terms of being able to select the method that’s most appropriate for their own clinical practice. Does the test mean you have a disease or not?” Homburger asks.
Moving Forward
Homburger, therefore, believes that “one of the greatest opportunities for improvement in the overall serology market would be improvement in standardization across the field.” Phadia is partnering with clinical investigators in the United States and around the world to develop a database of information that, if it does not drive standardization, it will at least enable physicians to use the tests practically and efficaciously.
At the same time, the company is also working to enhance serology testing by developing rapid antigen tests, component resolve diagnostics, and microarray technologies, particularly in the fields of allergy and autoimmune disease. “We can test for approximately 103 different components from 47 different allergens all on a single glass slide with 20 microliters of blood,” Homburger says.

To learn more about serology testing, search the CLP online archives.
Bio-Rad is focused on improving test performance (such as accuracy, turnaround time, etc) and clinical value through advanced technologies and automation. “[We are] developing tests to significantly improve clinical decision-making—for example, early-detection tests to quickly initiate treatment, specific targets for individualized oriented therapy, and multiplexing detection to establish a patient profile,” Madden says.
Alere’s intentions are similar to both Phadia and Bio-Rad, with an emphasis on faster turnaround through moderate complexity testing and automation. “Can some of these tests be driven to the point of care? Because, at the end of the day, not only do you want quality of results, but you want a faster turnaround time to so you can treat patients quicker,” Kolesar says. The concern impacts today’s serology products available now and those of the future.
Renee Diiulio is a contributing writer for CLP.