BD, Franklin Lakes, NJ, has received FDA market authorization for the BD Max vaginal panel, a first-of-its-kind molecular test to detect the most common causes for vaginitis.
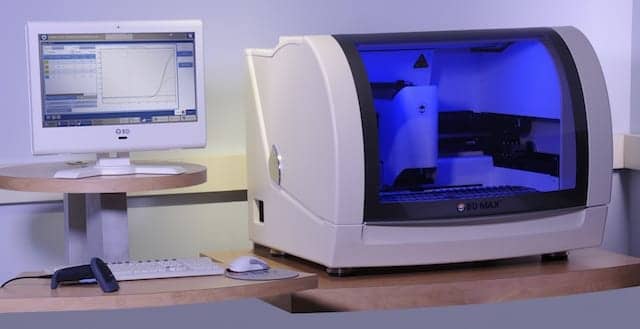
Laboratories and clinicians will now be able to use a single test to detect the microorganisms responsible for bacterial vaginosis (BV), trichomoniasis (TV), and vulvovaginal candidiasis (VVC), also known as a yeast infection, which are the most common infectious causes of vaginitis.1–3 The new in vitro diagnostic assay is the first multiplex, real-time polymerase chain reaction (PCR) assay authorized by FDA for the diagnosis of both vaginitis and vaginosis in women who exhibit symptoms of vaginal infection. BV diagnosis is especially challenging, as it is caused by bacterial imbalances in the vagina. To address this challenge, the BD Max vaginal panel has a unique algorithm that determines the ratio of healthy versus unhealthy bacteria, improving BV diagnosis.
“Vaginitis is highly prevalent, with large gaps in clinical management that improved diagnostics could help address,” says Mark Martens, MD, FACOG, chair of the department of obstetrics and gynecology at Jersey Shore University Medical Center, part of Hackensack Meridian Health. “Traditional methods used to detect vaginitis can be challenging due to the presence of many interfering substances in specimens, the large number of mixed infections, and the subjectivity of these methods. A multiplex microbiome-based real-time PCR assay has the potential to help clinicians improve patient management and help laboratories increase workflow efficiency.”
In the United States, vaginal infections result in more than 10 million office visits each year, with up to 75% of women experiencing at least one case of vaginitis (TV, VVC) or vaginosis (BV) in their lifetime.1,2,7 As many as half the women who suffer from a vaginal infection incorrectly assume it is a simple case of a yeast infection and attempt to self-treat with over-the-counter options before consulting a clinician.5
Additionally, inaccurate and inconsistent diagnosis of such conditions can leave up to 30% of women seeking treatment with the wrong diagnosis. Such erroneous diagnoses can lead to continued symptoms, repeat visits, inappropriate or missed treatments, and unnecessary associated healthcare system costs.2
In addition to causing irritating symptoms that reduce a woman’s quality of life, vaginal infections can have serious risks, including preterm or low birth-weight babies, late term miscarriage, and increased risk of transmitting or acquiring a sexually transmitted infection such as HIV or pelvic inflammatory disease (PID).3,4,6,7
FDA market authorization was granted under a de novo premarket notification (510(k)) petition, which is a regulatory pathway for novel products that are first-of-a-kind. The clearance represents the second addition to the BD reproductive and sexually transmitted infections portfolio within the past quarter. In September, BD obtained FDA clearance for the BD Max CT/GC/TV assay, which provides laboratories with the ability to detect chlamydia, gonorrhea, and trichomoniasis from a single specimen with one test.
“With FDA market authorization of the BD Max vaginal and CT/GC/TV panels, BD is now able to offer clinical laboratories automated PCR tests to aid in the detection and diagnosis of important reproductive and sexually transmitted infections, “ says Doug White, vice president and general manager for molecular diagnostics and women’s health at BD. “The US launch of the BD Max vaginal panel signifies BD’s continued commitment to elevating the standard of care for women’s health and sexually transmitted infections.”
For more information, visit BD.
REFERENCES
- Carr PL, Rothberg MB, Friedman RH, Felsenstein D, Pliskin JS. “Shotgun” versus sequential testing: cost-effectiveness of diagnostic strategies for vaginitis. J Gen Intern Med. 2005;20(9):793–799; doi: 10.1111/j.1525-1497.2005.0188.x.
- Hainer BL, Gibson MV. Vaginitis: diagnosis and treatment. Am Fam Physician. 2011;83(7):807–
- Sherrard J, Donders G, White D, Jensen JS. European (IUSTI/WHO) guideline on the management of vaginal discharge. Int J STD AIDS. 2011;22(8):421–429; doi: 10.1258/ijsa.2011.011012.
- Sobel JD. Vulvovaginal candidosis. 2007;369(9577):1961–1971; doi: 10.1016/S0140-6736(07)60917-9.
- Powell AM, Nyirjesy P. Recurrent vulvovaginitis. Best Pract Res Clin Obstet Gynaecol. 2014;28(7):967–976; doi: 10.1016/j.bpobgyn.2014.07.006.
- Lamont RF, Sobel JD, Akins RA, et al. The vaginal microbiome: new information about genital tract flora using molecular based techniques. 2011;118(5):533–549; doi: 10.1111/j.1471-0528.2010.02840.x.
- Powell K. Vaginal thrush: quality of life and treatments. Br J Nurs. 2010;19(17):1106–1111; doi: 10.12968/bjon.2010.19.17.78559.