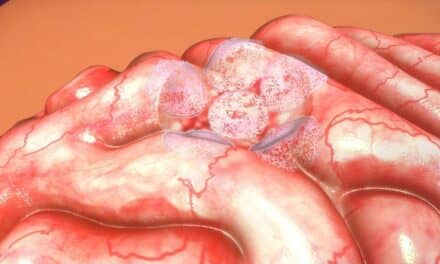
Early and accurate diagnosis of human prion diseases has been a long-standing difficulty, but in recent years the development of in vitro cell-free conversion techniques have extensively promoted the diagnosis of human prion diseases.
Currently, the definitive diagnosis of human prion diseases relies on pathognomonic histological features or PrPSc detection of patients’ brain tissue biopsy or autopsy samples, which is not feasible in most cases. But the development of the newer conversion techniques—such as technologies protein misfolding cyclic amplification (PMCA) and real-time quaking-induced conversion (RT-QuIC)—have improved diagnosis methods.
PMCA has high diagnostic accuracy in the blood, CSF, and urine samples of variant creutzfeldt–jakob disease (vCJD) patients. Again, RT-QuIC has high diagnostic accuracy for cerebrospinal fluid, olfactory mucosa, and skin samples of sporadic Creutzfeldt Jakob Disease (sCJD) patients. Applying these two technologies is of great significance to the early clinical diagnosis of human prion diseases and the reduction of blood-borne and iatrogenic transmission of prion.
Conversely, clinical diagnosis mainly relies on the combinations of the patient’s clinical symptoms. MRI and EEG are used to check for brain damage and detect surrogate markers such as the 14-3-3 protein in Cerebrospinal fluid (CSF), but this is often challenging.