By Luca Quagliata PhD, BCMAS
Summary:
Precision oncology is undergoing rapid transformation driven by next-generation sequencing (NGS) technology, but systemic barriers in testing access and trial enrollment must be overcome to realize its full potential in the fight against rising global cancer rates.
Takeaways:
- Explosive Growth with Urgent Challenges: Despite massive innovation and market growth in oncology, aligning the right therapy with the right patient remains a major barrier due to limited access and slow testing turnaround times.
- NGS as a Game-Changer: Decentralized, automated next-generation sequencing is revolutionizing clinical trials by enabling faster, broader patient access—particularly beyond large academic centers.
- Access = Impact: Democratizing molecular diagnostics is essential to scale precision oncology, accelerate clinical trial enrollment, and ensure equitable access to life-saving treatments.
Between 2019 and 2023, the oncology field witnessed an explosion of innovation with over 100,000 clinical trials launched; nearly one-third of those were dedicated to precision cancer therapies. This surge has not only opened new doors for patients but has also fueled the rapid growth of a high-value industry. The market was valued at $130 billion in 2023 and is projected to soar to approximately $350 billion by 2035.
This trajectory reflects a powerful shift: biomedical breakthroughs are no longer confined to just the lab and are now informing new therapies and reshaping the clinical landscape. At the center of this transformation is precision oncology, a discipline that is already delivering measurable gains and tangible improvement in patient outcomes.
However, despite this progress, one critical barrier persists: the ability to consistently and quickly align the right therapy with the right patient at the right moment. Solving this challenge is essential to unlocking the full promise of precision medicine and defining the future of cancer care.
It’s no secret that cancer incidences are on the rise at an alarming rate. Based on solid historical trends, the U.S. is projected to face an anticipated cancer epidemic by 2025, with over 2 million new oncology-related diagnoses and more than 600,000 cancer-related deaths expected.
Yet, despite this growing urgency and the global push toward widespread access to precision oncology solutions, clinical research is struggling to identify and enroll eligible patients into trials. Paradoxically, even as cancer cases increase, trial participation remains a significant bottleneck, presenting a harsh but undeniable reality.
To translate the promise of precision oncology into real-world impact, we must first confront the systemic barriers holding the industry back: low patient recruitment and retention, logistical challenges around tissue collection, and long turnaround times for genomic testing.
At first glance, these may seem like disconnected issues. But in truth, they point to a single, unifying challenge: the need to radically improve the efficiency and accessibility of genomic testing. Only then can we unlock the full potential of precision medicine and ensure that the right patients benefit from the breakthroughs they urgently need.
Time is of the Essence: The Evolving Role of NGS Testing in Precision Oncology Trial Efficiency
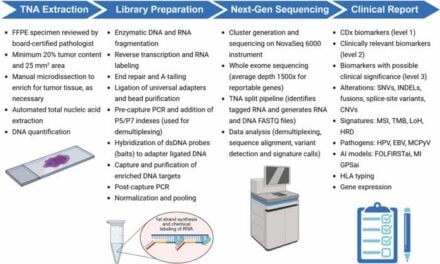
In clinical oncology research, the ability to move quickly is essential. Access to fast and reliable testing is critical for enrolling patients into clinical trials that could change their lives. This is where molecular testing via next-generation sequencing (NGS) comes into play. Traditionally, NGS adoption was constrained by manual, labor-intensive workflows and the need for specialized technical expertise. Oftentimes, these factors were only feasible for use at large academic centers while largely inaccessible to smaller, community-based hospitals.
But as clinical trials continue to face enrollment shortfalls, these very community centers represent an untapped opportunity to expand reach and bring research closer to where patients receive care. This is where we’re seeing a shift. Advances in sequencing technology and a broader industry recognition of the transformative power of precision medicine have enabled the rise of decentralized testing and consequent expansion of trial enrollment networks. Today’s innovative NGS solutions are designed for speed, simplicity, and accessibility and are aimed at delivering rapid, on-site testing without the traditional technical barriers.
This modernization is powered by automation. Processes that once required highly trained personnel can now run with minimal human input, from sample prep through to data analysis. As a result, turnaround times have been drastically reduced, making NGS a viable tool in a much broader range of clinical settings, including clinical research.
Rapid, decentralized NGS places research teams in the strongest position yet, allowing them to reach more patients, generate more inclusive and robust datasets, and accelerate enrollment without sacrificing sensitivity or scientific rigor.
The future of precision oncology depends on this more accurate, faster and more accessible molecular diagnostic technology.
Expanding Patient Access Through Ease of Use
Recent advancements in NGS have done more for cancer research than just making the technology easier to use. The growing availability of rapid NGS has begun to democratize precision medicine by providing features that allow for widespread adoption of this technology. Through these changes, we aim to make progress in ensuring as many patients and data points as possible are included in the research process, while also gaining a better understanding of how to fight a disease that affects so many people worldwide. The path is defined, now we must run towards the finish line.
Featured Image: Vladimir Efimov | Dreamstime.com
ABOUT THE AUTHOR

Luca Quagliata, PhD, BCMAS, is vice president and global head of Medical Affairs for Clinical Sequencing and Oncology at Thermo Fisher Scientific. Before joining Thermo Fisher, he worked as senior director for the R&D Unit as well as Leader of the Molecular Diagnostics team at the Institute of Medical Genetics and Pathology, care of the University Hospital Basel, Switzerland. Luca also served as a faculty member and was responsible for the Molecular Pathology curricula for the CAS – Certificate of Advanced Study in Personalized Molecular Oncology at the Faculty of Medicine, University of Basel.