PathogenDx’s UTI test is built on its D3 Array Platform. The multiplex test has a quick turnaround time with less waste—making it more economical for labs, and keeping the costs down for patients.
By Chris Wolski
With COVID moving from pandemic to endemic phase, testing providers have taken a hard look at the current needs of the market. This has resulted in filling the testing gaps caused by the pandemic.
As an individual example of the industry-wide trend, PathogenDx has taken its D3 Array Platform, which it used to successfully create COVID tests, and turned it to more routine, yet also important, urinary tract infections (UTIs).
CLP recently spoke with PathogenDx Co-founder and CEO Milan Patel about why the company is launching a UTI test, how it is keeping lab costs down, and how it is helping to improve testing access. Prior to co-founding PathogenDx, Patel spent over 25 years working with large public, small private, and entrepreneurial companies in numerous fields from the life sciences, to biotechnology, to government services, and the automotive industry.
Patel’s answers have been edited for length and clarity.
CLP: You are currently launching a UTI test. You’ve created tests for COVID among others. Why are you focusing on UTIs?

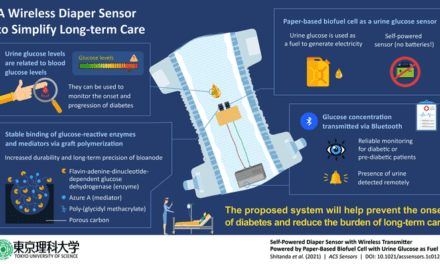
Milan Patel: At our core we are a pathogen diagnostics company. We look for bacterial, fungal, and viral contamination or infection. After successfully applying our technology to COVID and COVID variant testing, we took a hard look at other applications, specifically where multiple bacterial, fungal, or viral pathogens were the cause of infection. We wanted to find an area where our novel, multiplexing technology was a good fit and, more importantly, where we can positively impact the diagnostics paradigm of patient care and treatment. Looking at urinary tract infections, there are almost two dozen bacterial and fungal organisms or pathogens that can result in a UTI. In the present day, 30% of UTIs are considered to be ones with polymicrobial infections, or complicated UTIs—and we see about 10 to 11 million infections a year.
We took a hard look at what the technology we have invented, patented, developed, and commercialized in other markets does; the “Dynamic Dimensional Detection” or D3 Array is a multiplexing technology that has the capability to rapidly look at 100 targets in a single well test at a fraction of the cost, time and effort of conventional molecular methods. We quickly recognized that our technology is a fit for the type of complicated diagnostics present in UTI detection. PathogenDx has a unique opportunity to offer clinical labs access to a low-cost, high-throughput test with seamless automated data analytics and reporting, and no-waste on unused well technology. The D3 Array can look for multiple pathogens in the same test, simultaneously providing a comprehensive panel of causative agents and associated antibiotic resistance genes to aid in the diagnosis and treatment of complicated UTIs.
CLP: Can you explain how your D3 UTI test works?
Patel: Absolutely. The way that the D3 Array-UTI works is that a lab technician first takes a urine sample, and using standard magnetic bead extraction methods, extracts the pathogenic DNA cells in the sample that may be causing the infection. Out of the two dozen or so potential causative pathogens, is it E. coli? Klebsiella? Staphylococcus aureus? All three?
Next, you perform end-point PCR amplification to multiply the pathogenic DNA in that sample. We’re all familiar with PCR tests due to COVID testing. In the case of COVID, PCR was amplifying a viral DNA. In this case, it’s amplifying all the causative bacterial and fungal DNA in a sample.
The D3 Array-UTI utilizes a foil-sealed 96-well plate; once the DNA has been amplified, it gets dropped into the well. Each well contains the D3 Array, comprised of 390 probes, each of which has a specific genetic sequence that will be complementary to the single-stranded DNA of the bacterial or fungal species that have been amplified. If the causative pathogen is a strain of Klebsiella, that DNA strand in the sample will bind to the Klebsiella probes in the array, and it’ll bind very rapidly without the need for heating or cooling flow-cells. The difference here is each of the probes of the D3 Array are three-dimensional in nature, providing 100x greater binding surface area to bind amplicons (or single-stranded DNA) more rapidly and accurately, all at room temperature, delivering 100% specificity. Thereafter, the plate containing the D3 Array where the amplified DNA from the sample has binded to the probe(s) is then imaged, and an automated cloud-based software analyzes each and every probe—up to 390 per each well, and 96 wells in a plate—in less than one hour, without the need for human intervention.
That is the basic functionality of the test; the D3 Array acts as a sort of “net” to catch only the amplified DNA samples that are causing the infection very rapidly, very efficiently and very accurately.
CLP: One of the big benefits you’re providing is lower testing costs by running a single patient’s test in a single well. This seems to me to also be much more sustainable. Was this by design or an unintended benefit?
Patel: It was absolutely by design. When we think about what it means for a test like this to be sustainable, I think we also need to look at the unrelenting rise in the cost of healthcare—from insurance reimbursements decreasing to costs of technology to lab processing costs increasing. If this keeps going up, it will soon outstrip the ability for people to afford [testing], which will limit access. To counter this, we have invented a technology that possesses remarkable flexibility and affordability with the aim that as diagnostic testing evolves to require more content to inform treatment decisions, the technology can evolve alongside us without the need to scale on a one-to-one basis. .
The current standard practice is individual target testing; for example, if you’re testing a sample for ten pathogens, it would require the use of ten separate testing wells for each sample. If you’re looking for approximately two dozen potential different causative pathogens for a specific UTI, as well as twelve antibiotic resistance markers, you would be performing 36 separate tests each with their own specific primers or probe sites. This method is costly. We decided to put everything in one well in triplicate in an effort to converge and concentrate all of those individual targets in a single-well reaction, which helps us to completely flatten the cost of testing.
Further, [in the future] there will be additional pathogens that may cause infections, and additional antibiotic resistant genes that need to be tested. When additional test content is needed, our tests’ costs are not linear, they are fractional, and that is what sets PathogenDx’s technology apart from the standard multiplex serial qPCR panels that are currently being tested for UTIs. We can add more content to a given test at a fractional level to provide better economic efficiency and affordability—and thus, increased access sustainability.
CLP: Regular readers of CLP know that testing access is, for me, one of the most important challenges we’re facing today. You’re committed to testing access. Can you describe how the D3 UTI test provides more access?
Patel: When testing costs go up, access becomes limited to only those who can afford it. As I mentioned, we have created a test that is economical by design, but the other element we focused on was functional access. What that means is that specialized, proprietary equipment and service contracts required to conduct pathogen testing automatically limits the ability to have testing technology where it is needed most—like rural communities or developing nations.
Almost every lab in every country of the world had to get involved in COVID testing—PCR specifically. The D3 Array can be run off of standard molecular technology and lab equipment and doesn’t require service contracts for specialized equipment or maintenance contracts. It utilizes the standard liquid handlers and thermal cyclers that pretty much every molecular PCR lab in the world has, and standard sample extraction methods to extract the DNA out of the sample. Furthermore, anyone running COVID tests in a molecular lab can easily run our test without needing any additional training.
That’s what access means to us; not just for the patient but also to make the technology more widely available. Now, that’s not to say there are not still areas of the world where it will take time to implement this kind of technology—for example, a standard lab in a third world country or a developing nation may need additional equipment—but we are talking about standard PCR lab equipment, and this is something we are striving towards.
The final barrier for access we are trying to flatten is cost with respect to reporting. D3 Array test results are automatically captured via the cloud, so you’re not having to invest hours to analyze data like you have to with multiplex UTI qPCR panels to obtain your test results. D3 produces a report without all of the lab tech hours and costs that the syndromic qPCR panel has to go through to get the results from the instrument itself.
CLP: From the business perspective, what would you say are the primary benefits for a clinical lab implementing the D3 test?
Patel: From a business perspective, the primary benefits of implementing the D3 Array are cost, throughput, flexibility, and accuracy. The D3 Array costs significantly less than syndromic multiplexed qPCR panels with the same content, meaning 26 pathogens and 12 antibiotic resistance genes.
Beyond that, the D3 Array is capable of higher throughput compared to others, meaning the ability to run more samples per plate. There is no economic loss for unused wells, which is a really important distinction. If you only receive 30 patient samples daily, you lose the other 18 wells simply because you don’t have the samples to fill them. That’s the way that conventional technology works with syndromic qPCR panels. With our technology, our 96-well plate is foil-covered, and the foil is able to be cut for the precise number of wells being used in a given test, cutting both the cost and waste of unused wells. This is a big deal when you’re running a lab and cannot afford to be spending between $50-$60 per unused well because you don’t have the patient samples. Flexibility is incredibly important here.
Finally, the D3 Array features triplicate testing for detection and quantification of all pathogens and antibiotic resistance in a single well, and automatically reports all bioinformatic results to the cloud without needing any manual intervention. So, the level of accuracy is much better, with the controls built in.
CLP: What’s next for PathogenDx?
Patel: Great question. We fundamentally believe that one of the biggest challenges from a diagnostic standpoint—not just in the United States but globally—is access. From our perspective, the most important thing is to provide diagnostics that are accessible, affordable, and that address disease or infections, specifically in the women’s health diagnostics market.
That is what PathogenDx is focused on next; we are developing D3 Array tests for women’s health and STIs, specifically as a follow-on RUO test for clinical labs beyond UTIs that encompasses more comprehensive women’s health diagnostics.
Chris Wolski is chief editor of CLP.