At the beginning of January, the American Society for Colposcopy and Cervical Pathology (ASCCP) and the Society for Gynecologic Oncology (SGO) published a new interim professional guidance to help healthcare professionals determine how to best incorporate HPV primary screening into cervical cancer screening protocols.
The newly issued guidance, published simultaneously in Gynecologic Oncology, Journal of Lower Tract Genital Disease, and Obstetrics and Gynecology, supports HPV primary screening using an FDA-approved test in women 25 and older as an effective alternative to current screening recommendations with the Pap smear alone or cotesting with the Pap smear and HPV testing.1–3
The interim guidance was developed by ASCCP and SGO, with input from representatives of five other organizations, including the American Cancer Society (ACS), American College of Obstetricians and Gynecologists (ACOG), American Society for Clinical Pathology (ASCP), American Society of Cytopathology (ASC), and the College of American Pathologists (CAP).
Also published in Gynecologic Oncology at the beginning of the month, end-of-study data from the Addressing the Need for Advanced HPV Diagnostics (Athena) trial helped to inform the interim guidance report.4 Athena trial data showed that HPV primary screening using Roche’s Cobas HPV test detected significantly more cervical disease than a Pap test alone. A woman with a negative result from the Cobas HPV test had less than half the risk of developing cervical pre-cancer within 3 years than a woman with a negative Pap result.
“The interim guidance represents a new era in women’s reproductive health, particularly for younger women for whom clinicians have typically relied on testing with the Pap alone to detect cervical cancer,” says Alan Wright, MD, MPH, chief medical officer at Roche Diagnostics Corp, Basel, Switzerland.
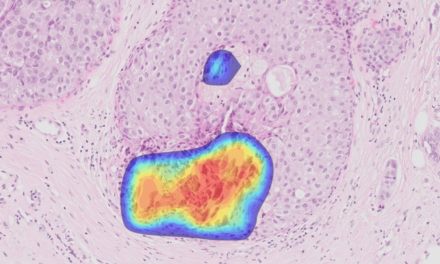
Persistent infection with human papillomavirus (HPV) is the principal cause of cervical cancer in women, with HPV implicated in greater than 99% of cervical cancers worldwide. According to the National Cancer Institute, there are more than 12,000 new cases of cervical cancer in the United States annually and 4,210 deaths due to the disease. The World Health Organization estimates there are more than 500,000 new cases of cervical cancer annually.
“The new end-of-study Athena data support the guidance recommendations for HPV as an acceptable option for first-line testing, because it shows that the Cobas HPV test had better negative predictive value than the Pap test, and increased sensitivity for the detection of pre-cancer—particularly in women aged 25 to 29,” Wright adds. “These data hold great promise for more effectively assessing a woman’s risk of cervical cancer, and we look forward to working with other professional societies as they develop official guidelines regarding use of the test as a primary screening tool.”
For the first time, the guidance provides clinicians the option to screen women 25 and older with an HPV test, prior to the Pap smear, to identify and stratify the risk of cervical disease before it progresses to cancer. The recommendation was informed by a review of 11 studies, including the Athena trial, a study of more than 47,000 women that showed an unexpectedly high burden of cervical disease in women aged 25 to 29.
Athena data demonstrated that more than one-third of all women with CIN3, the highest grade of cervical precancer, were aged 25 to 29. In addition, the trial found that Pap testing performed poorly in this age group, as more than 50% of the CIN3 or worse disease detected in women 25 to 29 by the Cobas HPV test was not detected by a Pap test.
Roche’s Cobas HPV test is currently the only HPV test approved by FDA for use as a first-line test in cervical cancer screening. It is also the only FDA-approved HPV test that provides specific genotyping information for HPV 16 and 18, the highest-risk types, while simultaneously reporting the 12 other high-risk HPV types as a pooled result—all in one run and from one patient sample.
The Cobas HPV test received FDA approval for use as a first-line primary screening test for cervical cancer in women 25 and older in April 2014. Prior to receiving the expanded indication, the Cobas HPV test was approved in April 2011 for screening patients aged 21 and older with abnormal cervical cytology results, and for use adjunctively with normal cervical cytology in women aged 30 and over to assess the presence or absence of high-risk HPV genotypes.
For further information, visit Roche Diagnostics.
REFERENCES
1. Huh WK, Ault KA, Chelmow D, et al. Use of primary high-risk human papillomavirus testing for cervical cancer screening: interim clinical guidance. Gynecol Oncol. 2015; available at http://dx.doi.org/10.1016/j.ygyno.2014.12.022.
2. Huh WK, Ault KA, Chelmow D, et al. Use of primary high-risk human papillomavirus testing for cervical cancer screening: interim clinical guidance. J Low Genit Tract Dis. 2015; available at http://dx.doi.org/10.1097/LGT.0000000000000103.
3. Huh WK, Ault KA, Chelmow D, et al. Use of primary high-risk human papillomavirus testing for cervical cancer screening: interim clinical guidance. Obstet Gynecol. 2015;125(2):330–337; available at http://dx.doi.org/10.1097/AOG.0000000000000669.
4. Wright TC, Stoler MH, Behrens CM, et al. Primary cervical cancer screening with human papillomavirus: end of study results from the Athena study using HPV as the first-line screening test. Gynecol Oncol. 2015; available at http://dx.doi.org/10.1016/j.ygyno.2014.11.076.