Two new American Cancer Society studies reveal significant increases in colorectal cancer screening rates and early-stage diagnoses among younger adults following updated screening guidelines.
Colorectal cancer screening among US adults aged 45-49 increased by 62% from 2019 to 2023, according to two studies published in the Journal of the American Medical Association that demonstrate the clinical impact of lowered screening age recommendations.
The screening surge has driven a corresponding 50% relative increase in local-stage colorectal cancer diagnoses in the same age group from 2021 to 2022, rising from 11.7 to 17.5 cases per 100,000 people. This represents a dramatic shift from 15 years of stable diagnostic rates in this population.
“These findings contrast with consistent increases of distant-stage diagnoses in this age group,” says Elizabeth Schafer, MPH, associate scientist at the American Cancer Society and lead author of the diagnostic study, in a release. “It is promising news because the uptick of cases is likely due to first-time screening in the wake of new recommendations for younger average-risk adults to begin testing for colorectal cancer earlier.”
The American Cancer Society lowered its recommended screening age from 50 to 45 in 2018, followed by the US Preventive Services Task Force in 2021.
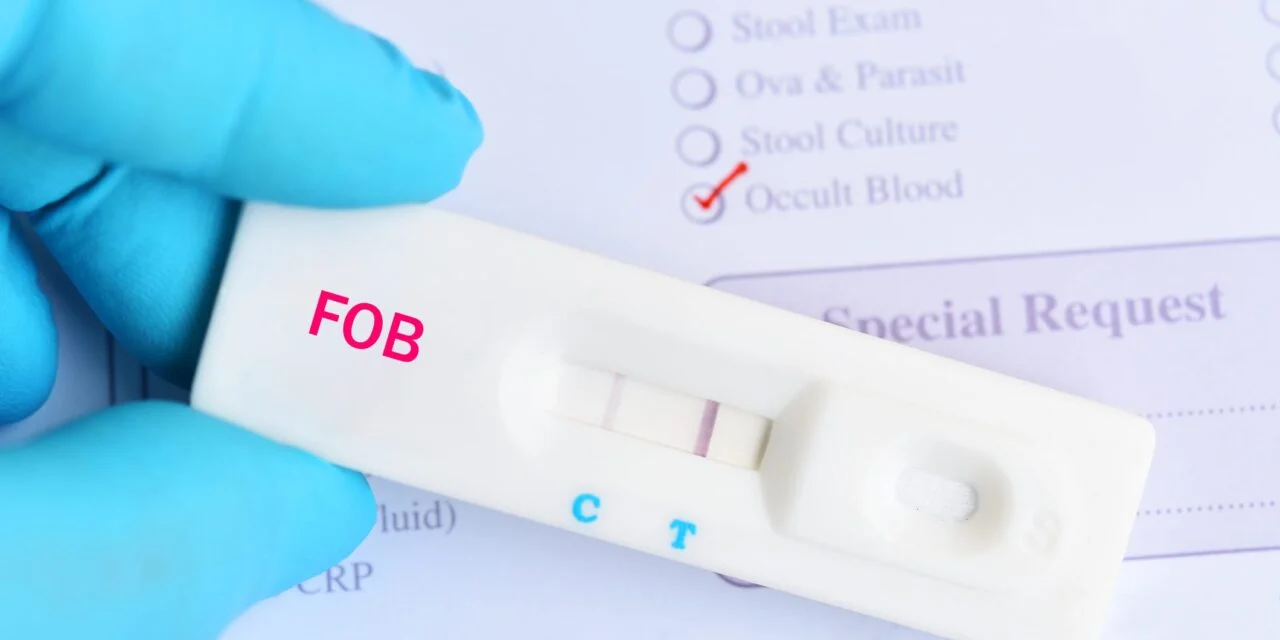
For clinical laboratories, the trend represents a significant shift in testing volume and demographics. Among 45-49-year-olds, colonoscopy screening increased by 43% while stool-based testing increased more than five-fold from 2019 to 2023.
The diagnostic study analyzed colorectal cancer cases from 2004 to 2022 among adults 20-54 years old across 21 geographic areas in the National Cancer Institute’s Surveillance, Epidemiology, and End Results program. Researchers found that while colorectal cancer incidence increased 1.1% annually from 2004 to 2019 in the 45-49 age group, the rate accelerated to 12% per year from 2019 to 2022.
The increase was driven primarily by detection of local-stage tumors, which increased 18.8% annually for colon cancer and 25.1% for rectal cancer from 2019 to 2022.
The screening study analyzed data from more than 50,000 individuals in the National Health Interview Survey, comparing colorectal cancer screening changes from 2019 to 2023 across multiple age groups.
However, screening disparities persist. Rates remained unchanged among individuals with less than a high school education and those without insurance, highlighting access barriers that could impact laboratory testing volumes in underserved populations.
“These studies further demonstrate the importance of people having access to comprehensive health insurance, which covers evidence-based preventive services,” says Lisa Lacasse, president of the American Cancer Society Cancer Action Network, in a release.
The second study’s lead author, Jessica Star, notes that while screening increases are encouraging, “screening for colorectal cancer in ages 45-49 remains suboptimal and has not increased equitably by both educational attainment and insurance status.”
For laboratories, the findings suggest continued growth in colorectal cancer screening test volumes, particularly stool-based assays, as healthcare providers implement the updated age recommendations across diverse patient populations.
ID 123833462 © Jarun011 | Dreamstime.com