Circulating tumor cell analysis showed 85% sensitivity and 100% specificity for predicting tarlatamab treatment benefit in small cell lung cancer patients.
Researchers at Mass General Brigham Cancer Institute have developed a blood test that can predict which patients with small cell lung cancer will benefit from the recently approved immunotherapy drug tarlatamab, potentially eliminating the need for invasive tissue biopsies to guide treatment decisions.
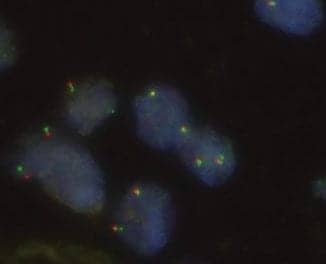
The test analyzes circulating tumor cells in blood samples to detect levels of DLL3, a neuroendocrine marker that tarlatamab targets. In a study of 20 patients, published in Cancer Discovery, the blood-based test correctly identified 85% of patients who experienced clinical benefit from tarlatamab and 100% of those who did not respond to treatment.
“Isolating cancer cells from the blood has tremendous potential to guide immune-related cancer therapies, and our group has created cutting edge bioengineering technologies for purification of these circulating tumor cells,” says Daniel A Haber, MD, PhD, director of the Krantz Family Center for Cancer Research at the Mass General Brigham Cancer Institute and senior author of the study, in a release. “We’ve learned a lot about the biology of these cells, but we haven’t had a test that has direct clinical relevance. In this study, we believe that we achieved this.”
Addressing Treatment Response Variability
Tarlatamab received full FDA approval in late 2025 for treating small cell lung cancer after prior chemotherapy. The bispecific antibody works by recruiting T cells to attack cancer cells that express DLL3. However, about half of patients experience cancer progression within six months of starting therapy.
While clinicians previously assumed that all small cell lung cancer cases express DLL3, the researchers found that only half of the patients in their study had abundant DLL3-positive cancer cells circulating in their blood. These patients were the ones who responded to tarlatamab treatment.
The findings suggest that current assumptions about DLL3 expression in small cell lung cancer may be incorrect, and that blood-based testing could provide a more accurate assessment of which patients will benefit from DLL3-targeted therapies.
Clinical Implementation Potential
The blood cell enrichment technology used in the study has been licensed to TellBio Inc, suggesting potential commercial development of the diagnostic test. The noninvasive nature of blood testing could make treatment selection more accessible compared to tissue-based biomarker testing, which requires invasive procedures.
“Our work may help predict which patients with SCLC are likely to respond to tarlatamab and potentially other antibodies targeting DLL3, many of which are in development,” says Justin Gainor, MD, program director of the Center for Thoracic Cancers at the Mass General Brigham Cancer Institute and co-corresponding author, in a release. “It also has potential implications for other cancers that express DLL3 as they become more aggressive and for the field of antibody-directed cancer therapies.”
ID 2783120 © Pmisak | Dreamstime.com