Summary: The College of American Pathologists collaborated with several organizations to develop evidence-based recommendations for testing immunotherapy biomarkers, such as Programmed Cell Death Ligand-1 (PD-L1) and tumor mutation burden (TMB), in patients with non-small cell lung carcinoma (NSCLC).
Takeaways:
- The recommendations from CAP were developed in collaboration with organizations such as the International Association for the Study of Lung Cancer, the Pulmonary Pathology Society, the Association for Molecular Pathology, and the LUNGevity Foundation.
- Immunotherapy has emerged as a promising treatment option for NSCLC patients, but its effectiveness varies among individuals. PD-L1 expression and tumor mutation burden (TMB) serve as clinically validated biomarkers that can help predict response to immune checkpoint blockade therapies.
- The guideline acknowledges the technical challenges associated with PD-L1 testing, including the development of divergent companion diagnostic PD-L1 tests and the widespread use of laboratory-developed tests (LDTs) due to cost and access limitations.
The College of American Pathologists (CAP) developed evidence-based recommendations for the testing of immunotherapy biomarkers, including Programmed Cell Death Ligand-1 (PD-L1) and tumor mutation burden (TMB) in patients with non-small cell lung carcinoma (NSCLC).
CAP Collaborating on Immunotherapy Biomarkers
The recommendations from CAP were done in collaboration with the International Association for the Study of Lung Cancer (IASLC), Pulmonary Pathology Society (PPS), Association for Molecular Pathology (AMP) and the LUNGevity Foundation.
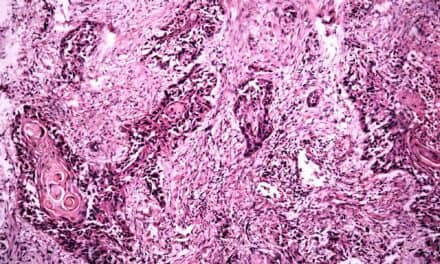
Use of PD-L1 and TMB Testing for NSCLC Patients
“Many lung cancer patients may benefit from therapies that can harness the immune system, including anti-PD-1 or PD-L1 therapies. However, the benefit of these therapies is not universal, and clinically validated biomarkers that can help predict response include PD-L1 expression and proposed tumor mutational burden (TMB),” says Larissa Furtado, MD, FCAP. “This guideline is intended to provide an overview of the clinical rationale for the use of PD-L1 and tumor mutational burden (TMB) testing for patients with non-small lung cancer. It highlights the technical challenges of PD-L1 testing and interpretation, including some of the complexities introduced by the development of divergent companion diagnostic PD-L1 tests for different immune checkpoint blockade therapies. It outlines the rationale for use of TMB and the current limitations of this test for lung cancer patients.”
PD-L1 IHC Antibodies and Assays
This guideline, now available in an early online release in the Archives of Pathology & Laboratory Medicine, was driven by the production of PD-L1 assays and scoring criteria that have evolved with individual therapies. At the same time, for reasons of cost and access, PD-L1 IHC antibodies and assays developed outside of the scope of randomized controlled trials have garnered widespread use.
“Clinical trials have demonstrated that drugs that block Programmed Cell Death 1 (PD-1), and PD-L1 lead to significant improvements in both response and survival relative to conventional cytotoxic chemotherapy for patients with advanced stage NSCLC,” says guideline update co-chair Lynette Sholl, MD, FCAP.
The expert panel recognized that the regulatory-approved diagnostics are clinically validated, and as such their use is recommended. However, most laboratories may be relying on laboratory developed tests (LDTs) because of limited access to a full suite of approved clones and platforms, as well as the increased cost of running companion diagnostic-labeled assays.
“To ensure patient access to PD-L1 testing, particularly at the local level, we endorse the use of LDTs and validated PD-L1 IHC (LDTs) following technical validation against one or more of the approved companion diagnostic PD-L1 assays,” says Furtado.
Further reading: Blood Tests Identify NSCLC Patients Who May Benefit from Immunotherapies
PD-L1 Testing of Patients with Lung Cancer
With six recommendations, the guideline provides data and details regarding the efficacy and utility of PD-L1 testing of patients with lung cancer. This new guideline was developed by IASLC, PPS, the LUNGevity Foundation and the CAP Center, which develops evidence-based guidelines and consensus statements related to the practice of pathology and laboratory medicine. Through this work, the CAP and its members continually improve the quality of diagnostic medicine and patient outcomes.