A new prostate cancer screening method could help doctors better predict which patients need to undergo a biopsy, reducing unnecessary procedures.
By Arnon Chait, PhD, MBA
Summary: A new prostate cancer screening method using protein structure-based biomarkers can help doctors better predict which patients need biopsies, reducing unnecessary procedures.
Takeaways:
- Overdiagnosis and Overtreatment: Current prostate cancer screening methods often lead to unnecessary biopsies, contributing to significant healthcare costs and patient stress.
- Protein Biomarkers: The IsoPSA test, which detects cancer-specific structural changes in PSA proteins, offers higher specificity and a lower false positive rate than traditional DNA or RNA-based tests.
- Clinical Impact: Studies show that IsoPSA can significantly reduce unnecessary biopsies while ensuring patients with high-grade prostate cancer receive appropriate care.
Prostate cancer is the second most common cancer in men, with one in eight receiving a diagnosis in their lifetime.1 And yet, as prevalent as this cancer is, the current methods for detection and diagnosis tend to result in the overtreatment of patients, costing the health care system millions of dollars via inaccurate tests and unnecessary biopsies.
Here, we’ll explore how the current standard of care is causing tremendous waste in health care spending and how new screening tests based on protein structure-based biomarkers may help doctors better determine which patients are at lower risk of having high-grade prostate cancer and, therefore, reduce referrals for prostate biopsies.
Prostate Cancer Screening: Striking a Delicate Balance
First, let’s take a step back. When it comes to cancer tests, a delicate balance must be struck: Prostate cancer screening must detect cancer early, before it spreads when it’s easier to treat, but should also limit overdiagnosis and overtreatment where further testing and treatment can cause more harm than good.
For example, intervening if the patient does not actually have cancer, or if the tumor is low-grade and will likely remain asymptomatic and not life-threatening during the patient’s lifetime. Overdiagnosis and overtreatment are significant in prostate cancer, where, according to one study, the current screening protocols lead to unnecessary biopsies and overdiagnosis of as many as 60% of men.2
Doctors need better screening protocols and methods to increase the accuracy of prostate cancer screening, thereby reducing excess testing triggered by the current standard of care.
Wasted Spending Resulting from the Current Standard of Care
There’s no clear consensus on which patients doctors should screen for prostate cancer. However, the general approach is to screen select men 55-69 years old based on individual risk factors and patient preferences.3 Ultimately, it’s not recommended to screen patients over 70 since there is a significant risk of overdiagnosis, and little evidence suggests that screening this demographic increases survival rates.
Screening typically begins in a primary care setting with a prostate-specific antigen (PSA) test to measure PSA levels in the blood. Generally, elevated PSA levels, ≥4 ng/mL, can indicate an elevated risk for high-grade prostate cancer. On the other hand, it could also be the result of something more benign, such as benign prostatic hyperplasia, recent exercise, inflammation of the prostate, or even recent sexual activity. With this lack of clarity, it’s no surprise that the PSA test produces numerous false positive results.
If initial PSA levels come back elevated, the primary care physician may refer the patient to a urologist who may order additional tests, such as screening tests and imaging tests, to try to assess cancer risk and visualize potential abnormalities in the prostate.
If these tests do not rule out the possibility of cancer, then the urologist will often order a prostate biopsy to establish the diagnosis. However, this process is far from perfect. Although about $1.8 billion is spent on PSA testing and $3 billion on prostate biopsies in the United States per year, only about 25% of men who had an elevated PSA result triggering a biopsy are diagnosed with high-grade prostate cancer; all others underwent unnecessary biopsies that either came back normal or indicated low-grade prostate cancer that didn’t require treatment.4,5,6 Importantly, it’s not just about the money. This high false positive rate also results in potentially significant complications such as sepsis, and puts undue stress on otherwise healthy patients, who spend months wondering if they have cancer as they go through the (sometimes invasive) diagnostic process. There’s no question that the current standard of care is due for an upgrade.
Emerging Diagnostics: DNA and Protein Biomarkers
Following an elevated PSA test result, physicians have several options for follow-up testing, such as an ancillary test to assess the patient’s risk of having high-grade cancer. Many of these tests look for cancer biomarkers in DNA or RNA in blood or urine.
However, the results of these tests do not always give doctors clear answers, require specialized technology to perform, and need an expert eye to interpret their results. Moreover, mutated DNA or RNA doesn’t necessarily mean that cells are actually producing altered proteins; it simply indicates that the genetic blueprint for cancer may be present. DNA- and RNA-based tests may also not be sensitive enough to detect low levels of biomarkers in the blood or urine if the disease is at an early stage. An ideal biomarker should be defined as close to the underlying disease process, namely, should be detected only if, for example, high-grade prostate cancer actually exists.
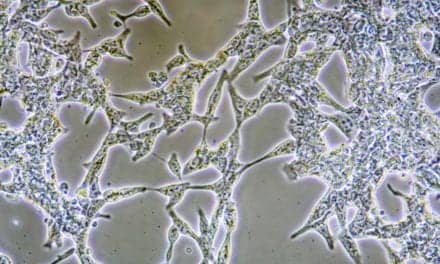
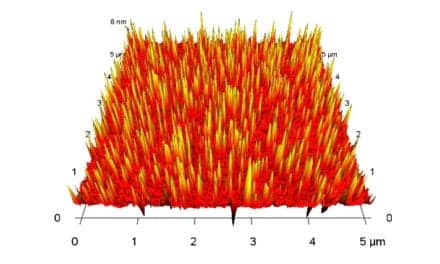
Doctors now have a new option: an emerging diagnostics technology that assesses modified isoforms of PSA protein in the patient’s blood. The test, called IsoPSA, can better stratify a patient’s risk for prostate cancer and better inform decisions regarding which patients should undergo a biopsy. The changes detected by the test result from alterations in protein structure, glycosylation, and protein-protein interactions that are known to be directly correlated with cancer, and therefore, unlike DNA and RNA biomarkers, are a more direct indicator of the presence of cancerous cells. The test uses an aqueous two-phase system to partition and detect these cancer-specific structural isoforms of PSA into two adjacent specially designed aqueous phases. Recent studies indicate that this approach is as sensitive at detecting cancer as the standard of care but offers significantly higher specificity, resulting in a lower false positive rate—meaning that doctors can use it to screen out patients who are unlikely to have high-grade prostate cancer and therefore need not undergo a biopsy.
Several studies highlight the power of a test like IsoPSA. In one study of 207 patients—22% of whom had clinically significant prostate cancer—the test looking for PSA isoforms combined with imaging most accurately predicted the risk of having clinically significant prostate cancer.7 In another study of 734 men with elevated PSA levels (≥4 ng/ml), testing PSA isoforms resulted in a 55% net reduction in recommendations for prostate biopsy and a 9% reduction in recommendations for magnetic resonance imaging.8
Thus, in a real-world clinical setting, doctors readily adopted the test to reduce the number of unnecessary biopsies they performed while ensuring biopsies are performed on the right patients.
How Better Prostate Cancer Screening Could Impact Men’s Health Care
Testing for PSA protein isoforms helps bridge the gap between elevated PSA levels and invasive biopsies. This novel blood test provides information to support decision-making between doctors and patients, enabling doctors to reassure patients who don’t need biopsies and guiding those who do.
The data are clear. This new prostate cancer testing method could reduce the amount of overdiagnosis and overtreatment in the men’s health sector, reducing wasteful spending while ensuring patients at high risk get the care they need.
About the Author

Arnon Chait, PhD, MBA, is the chief executive officer of Cleveland Diagnostics. An entrepreneur, scientist, and educator, Chait’s extensive multidisciplinary background spans physics, engineering, and bioscience. As Cleveland Diagnostics’ CEO, he applies his vast experience commercializing innovative science to drive the company’s vision of bringing early cancer detection into everyday practice with advanced testing that is more simple, accurate, and cost effective than current options.
References
- American Cancer Society. Key Statistics for Prostate Cancer. Last Revised January 19, 2024. Accessed July 23, 2024. https://www.cancer.org/cancer/types/prostate-cancer/about/key-statistics.html#:~:text=About%201%20in%208%20men,to%20develop%20in%20older%20men.
- Welch HG, Black WC. Overdiagnosis in cancer. J Natl Cancer Inst. 2010;102(9):605-613. doi:10.1093/jnci/djq099
- Centers for Disease Control (CDC). “Should I Get Screened for Prostate Cancer? Prostate Cancer. Published Oct. 16, 2023. Accessed July 18, 2024. https://www.cdc.gov/prostate-cancer/screening/get-screened.html?CDC_AAref_Val=https://www.cdc.gov/cancer/prostate/basic_info/get-screened.htm
- Ekwueme DU, Stroud LA, Chen Y. Cost analysis of screening for, diagnosing, and staging prostate cancer based on a systematic review of published studies. Prev Chronic Dis. 2007;4(4):A100.
- Ablin RJ. “The Great Prostate Mistake.” The New York Times. Mar 9, 2010. Accessed July 18, 2024. https://www.nytimes.com/2010/03/10/opinion/10Ablin.html
- National Institutes of health. “Prostate-Specific Antigen (PSA) Test.” National Cancer Institute. Updated Mar. 11, 2022. Accessed July 18, 2024. https://www.cancer.gov/types/prostate/psa-fact-sheet
- Benidir T, Lone Z, Wood A, et al. Using IsoPSA With Prostate Imaging Reporting and Data System Score May Help Refine Biopsy Decision Making in Patients With Elevated PSA. Urology. 2023;176:115-120. doi:10.1016/j.urology.2023.03.014
- Scovell JM, Hettel D, Abouassaly R, et al. IsoPSA® Reduces Provider Recommendations for Biopsy and Magnetic Resonance Imaging in Men with Total Prostate Specific Antigen ≥4 ng/ml: A Real-World Observational Clinical Utility Study. Urol Pract. 2022;9(2):173-180. doi:10.1097/UPJ.0000000000000291