 |
Some in the medical community think pharmacogenomics will have such a pervasive impact on medicine that it will result in at least one additional medical specialty—genomic medical practitioners. Others think that pharmacogenomics—personalized medicine—will be so integrated throughout health care that it will be as prevalent as a stethoscope or blood pressure cuff. What isn’t being debated is that pharmacogenomics will have a significant impact and that it will influence the way health care is delivered in the not-too-distant future.
That will be especially evident in the clinical laboratory, where much of the science behind pharmacogenomics will occur. “We already offer a fairly extensive menu of these tests, and we have seen increasing usage,” says Myla Goldman, MD, executive vice president, chief scientific officer, and medical director for Laboratory Corporation of America (LabCorp), Burlington, NC. “I anticipate seeing the menu expand further and usage continue to increase.”
Carol Reed, MD, chief medical officer of Clinical Data Inc, Newton, Mass, concurs. “In tomorrow’s world, we will have a broad array of tests physicians can use to guide them across the spectrum of drugs when initiating therapy for a disease or changing therapy in response to new illnesses,” she says.
The volume will mean challenges and opportunities for laboratories. Because each drug is different, the tests will be different. Technologies and platforms may differ. And parameters, profiles, results, and interpretation will differ as well. Laboratories will be the key to providing information physicians can use. But, according to James A McClintic, CEO of Exagen Diagnostics Inc, Albuquerque, NM, test developers will also play a role.
 |
| Pharmacogenomics is expected to have a big impact on the clinical lab, increasing volumes and opportunities. |
Exagen’s marketing and distribution plans for future pharmacogenomics tests include physicians. “The inventor of the test must educate the physician about the utility of the test,” McClintic says. “We will not hold an exclusive relationship with laboratories, but will go directly to physicians to talk about our products. They want to be educated, and they want better tests.”
Better Tests
Pharmacogenomics holds the promise of better tests, with advantages related to improved treatment and greater safety. The diagnostics assist treatment decision making in multiple ways, including efficacy, safety, dosing, and prognosis.
Efficacy simply refers to whether a specific drug will work in a particular patient. Goldman uses HercepTest by Dako, Carpinteria, Calif, as an example. The test is a semiquantitative immunohistochemical assay that determines overexpression of HER2 protein in breast cancer tissues, with indications for possible herceptin therapy.
“In this situation, all patients would receive this test to determine if the drug even has the potential to work in the patient,” Goldman says. “Do they have the receptors that will respond to the drug?”
If the patient does not have the receptors, the physician will choose an alternative treatment with a greater chance of working, avoiding the potential side effects and wasted time of an unsuccessful trial with herceptin.
Pharmacogenomics can also help to avoid adverse effects in general. Goldman predicts that doctors will weigh the risk of an adverse event against its effects as well as how well the patient could tolerate it. “If an adverse effect is liver toxicity, and a patient has underlying liver disease, this will impact the physician’s decision making,” Goldman says.
“These tests can provide information about a patient’s ability to metabolize a drug, and therefore, what their exposure to the drug might be,” Reed says.
CLDI offers three such tests: PGxPredict:Clozapine, which determines the risk of developing agranulocytosis in response to clozapine treatment for refractory schizophrenia; PGxPredict:Rituximab to predict response to Rituximab monotherapy in patients with follicular, CD20-positive B-cell non-Hodgkin’s lymphoma; and PGxPredict:Warfarin, which can help to avoid bleeding by maximizing the drug’s dose efficacy.
Warfarin testing is also an example of the role pharmacogenomics can play in dosing. “Warfarin is an anticoagulant used to treat people with heart disease, stroke, and the like,” says Steven Seelig, MD, PhD, divisional vice president, research, for Abbott Molecular, Des Plaines, Ill. “There are population differences in how the drug is metabolized and the resulting toxicity and risk of adverse events. Slow metabolizers have a greater risk of suffering a bleeding event.”
 |
| Pharmacogenomic test results are of tremendous economic value to clinical labs, and to the health care system as a whole. |
Testing can help guide dosing decisions, though Seelig notes that it is not the only factor a physician takes into consideration. He suggests that factors such as diet and other medications can modify the ability to predict warfarin response.
“Clinicians can use pharmacogenomic tests as one of their options. They allow the physician to individualize his or her approach to the patient,” Goldman says. “When there is a more urgent need to get the maximal drug benefit as soon as possible, pharmacogenomic testing can allow maximizable dose.”
Pharmacogenomic testing can also offer individualized prognostic information that can impact treatment. Exagen Diagnostic’s eXagenBC is designed to determine the risk of recurrence in breast cancer patients. Knowing this risk may influence a particular course of treatment. “These tests provide more knowledge about the disease,” McClintick says.
Enhanced Care
Exagen filed the test with the FDA in early April for approval as an in vitro diagnostic kit. Pharmacogenomics is still a new discipline, and specific regulation is limited, but rules impacting the clinical laboratory and medical devices still apply. FDA-cleared tests provide the benefit of validation.
 |
| The PathVysion HER-2 DNA Probe Kit is approved by the FDA to determine HER2/neu gene amplification in breast cancer patients. The cutoff for herceptin treatment has been established through significant clinical trials. |
“It can be hard for an individual laboratory to collect the data that shows the test is delivering the desired performance,” Seelig says.
The FDA may also mandate a test’s use through a drug’s labeling requirements. Labels for tamoxifen, warfarin, and herceptin have been modified to incorporate pharmacogenomic indications. “If there is anything to be gained, the FDA wants to label all drugs with pharmacogenomic requirements and is trying to be proactive and encouraging in this area,” Seelig says.
Parameters can vary with the clinical setting. “As in many aspects of medicine, they vary depending on the patient and the setting,” LabCorp’s Goldman says. “For example, if a patient is hospitalized, physicians might be able to use observation to watch a patient for an adverse drug reaction, but if patients are being sent home, they may choose to test them beforehand. If there is a choice, the test may be more cost-effective than hospitalization.”
Guidelines—those already developed and those in development—can provide further recommendations, not only on when to perform the tests but also on how to interpret them. “A raw genetic marker is not helpful to most physicians,” CLDI’s Reed says. “It’s the interpretation the physician needs to see. Is the patient more or less likely to experience an adverse event?”
Goldman concurs, but adds: “Most of the time, we are not so specific as to say you should give this patient this exact dosage, because we may not know every parameter that is relevant to that patient. But we can suggest the physician increase the dosage over the usual level because the patient is a rapid metabolizer of the drug.”
Validated clinical trials can help to create standards that guide results-based recommendations. Abbott’s PathVysion HER-2 DNA Probe Kit, approved by the FDA, employs a fluorescence in situ hybridization (FISH) platform to determine whether the HER2/neu gene is amplified in breast cancer tissue samples. The cutoff, according to Seelig, has been established through significant clinical trials. “If a patient’s amplification is above a certain point, she is eligible for herceptin treatment,” Seelig says.
Clear results permit the physician to understand how to incorporate the tests into the patient’s care management. Physicians have a responsibility to know this information, but in reality, it can be difficult to always be up to date.
“Labs play a really important role in providing accurate communication in the interpretation of results as well as caveats, test validity, and relative risks,” Seelig says.
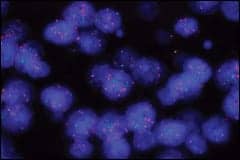 |
| Fluorescence in situ hybridization (FISH) is a popular platform for pharmacogenomic tests. Here, the technology is used in eXagenBC to determine hormone receptors in breast cancer patients. |
Promise and Opportunity
Of course, providing such detailed data will require more resources, particularly since there is a variety of platforms. Popular platforms include real-time polymerase chain reaction, FISH, and flow cytometry, but even these can be expensive to offer, McClintic notes.
“The rapid advancement and development of technology and platforms in this area could potentially pose a burden in terms of multiple tests coming from multiple manufacturers on multiple platforms,” CLDI’s Reed says. “The capital investment required to stay on top of the technology can be high.”
Volume will determine which tests are economically feasible to run in-house and which need to be sent out. “In some cases, the tests are so rare, they may be ordered only once a month,” McClintic says. “Keeping these tests validated can be a resource robber.”
However, the tests offer a considerable opportunity for laboratories. McClintic suggests that recent acquisitions in the industry are indicative of larger laboratories positioning themselves in a soon-to-be burgeoning market.
“Pharmacogenomics is a growth area for clinical laboratories,” Seelig says. “If they can generate these test results that are of tremendous economic value to the health care system as a whole, they will be compensated accordingly. It’s a path for clinical labs to generate useful business.”
 |
| For more information, search for “pharmacogenomics” and “genetic testing” in our online archives. |
Being useful is key in introducing these tests. McClintic refers to Exagen research indicating that very few tests are ordered when there is no therapy available. “If there isn’t a treatment available, the test is no good,” McClintic says. He suggests that testing is slightly ahead of therapeutics.
Eventually, however, the two will catch up. At that point, we might know whether pharmacogenomics will branch into its own specialty or become all-pervasive; either way, expect it to bring better tests and enhanced care.
Renee DiIulio is a contributing writer for CLP.
Pharmacogenomics and Everyday Health
Pharmacogenomic testing is not yet prevalent throughout the health care industry, but experts expect personalized medicine to become an influential wave of the future. Once that happens, pharmacogenomics will become so routine that the tests will be used to tackle everyday health concerns, such as quitting smoking.
Researchers worldwide are analyzing the role that pharmacogenomics can play to help achieve this often elusive goal. “The hope is that it would reveal the optimal treatment in terms of the dosage and the length of treatment,” says Marcus Munafo, PhD, lecturer in the department of experimental psychology at the University of Bristol, UK.
There are a number of potential medications approved by the FDA for smoking cessation. They include varenicline, buproprion, and nicotine-replacement therapies such as the patch, gum, inhaler, nasal spray, and lozenges.
Munafo suggests that when utilized during an initial visit for smoking cessation, pharmacogenomic tests could reveal patient specifics in two areas: the response to a drug or the drug’s potential efficacy, and the presence of a marker for dependence. “This would be a more intrinsic character of the individual, but could indicate the need for a higher level of medication,” he says.
Turnaround would work best within a few days, but it would be a challenge to the lab. Results would be interpreted by clinicians using decision-making algorithms. It is likely that a broad spectrum of patient characteristics would need to be considered in determining treatment, which would include choosing the drug, the dose, and the length of treatment. “A physician may find that one patient will fare better with one therapy rather than a combination,” Munafo says.
Of course, the tests will have to prove their value before their use becomes widespread, particularly in countries such as the UK that have socialized medicine. “It’s not clear the actual cost will be outweighed by the benefits in treatment,” Munafo says, “which is a research issue that will have to proceed in parallel with the actual science.”




