NeoGenomics,a provider of oncology testing and global contract research services, announced results of a new study of the RaDaR assay in patients with muscle-invasive bladder cancer immediately following treatment with a combination of the immune checkpoint inhibitors in the neoadjuvant setting. Plasma and urine collected from the patients during treatment was analyzed.
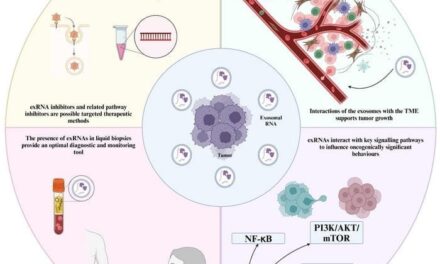
The RaDaR assay is a personalized, highly-sensitive sequencing test for the detection of minimal residual disease (MRD) and recurrence. MRD is the trace amounts of circulating tumor DNA (ctDNA) that remain after surgery or other cancer treatment. The study, published in the journal Nature Medicine, found that the absence of ctDNA in plasma—as detected by RaDaR—was associated with patient responses to treatment prior to surgery offering the possibility of avoiding aggressive surgery that removes the patient’s bladder (also known as a cystectomy).
“Most patients with muscle-invasive urothelial cancer are at a high risk for recurrence and most will undergo cystectomy that results in the removal of the bladder,” says Vishal Sikri, president, Advanced Diagnostics, NeoGenomics. “If possible, preserving a patient’s bladder is clearly an important outcome if new approaches to neoadjuvant treatments are successful. By determining if a patient has responded well to neoadjuvant treatment, RaDaR provides necessary insights to help oncologists decide whether a patient may be a candidate for bladder-sparing treatment strategies.”
The new data are part of the second cohort of the Phase 1b/2a NABUCCO (Neo-Adjuvant Bladder Urothelial Carcinoma Combination-immunotherapy) trial, which investigated patient responses to neoadjuvant treatment with a CTLA-4 inhibitor (ipilimumab) in combination with a PDL1 inhibitor (nivolumab) among patients with locoregionally-advanced urothelial cancer. In both cohorts, RaDaR assay was used before and during neoadjuvant therapy as well as pre-surgery to assessed ctDNA in urine and blood plasma to determine patient response to treatment.
Cohort 1 (n=24) helped establish the feasibility of neoadjuvant therapy with ipilimumab 3 mg/kg plus nivolumab 1 mg/kg, demonstrating high pCR rates (a secondary endpoint). In Cohort 2 (n=30), patients received either ipilimumab 3 mg/kg plus nivolumab 1 mg/kg (cohort 2A) or ipilimumab 1 mg/kg plus nivolumab 3 mg/kg (cohort 2B), both for two cycles, followed by nivolumab 3 mg/kg.
Overall, 43% (6 patients) in cohort 2A and 7% (1 patient) in cohort 2B achieved a complete pathological response (pCR), the primary endpoint. The absence of ctDNA in blood plasma was highly associated with both pCR (odds ratio (OR): 45.0, 95% CI: 4.86-416.46) and PFS (hazard ratio (HR): 10.4, 95% CI: 2.86-37.50). In urine, the absence of ctDNA was linked to pCR but not PFS.
“Although cisplatin-based chemotherapy plus radical cystectomy remains the currently recommended treatment for muscle-invasive bladder cancer, there are some patients who are not eligible to receive chemotherapy and the prognosis for this patient population is poor,” says Shashikant Kulkarni, chief scientific officer, NeoGenomics. “The findings from the NABUCCO trial offer initial evidence in hopefully improving the outlook for these patients. Importantly, the research shows that the RaDaR assay can be used successfully to guide decision-making and help oncologists personalize patient care based on their risk of recurrence.”
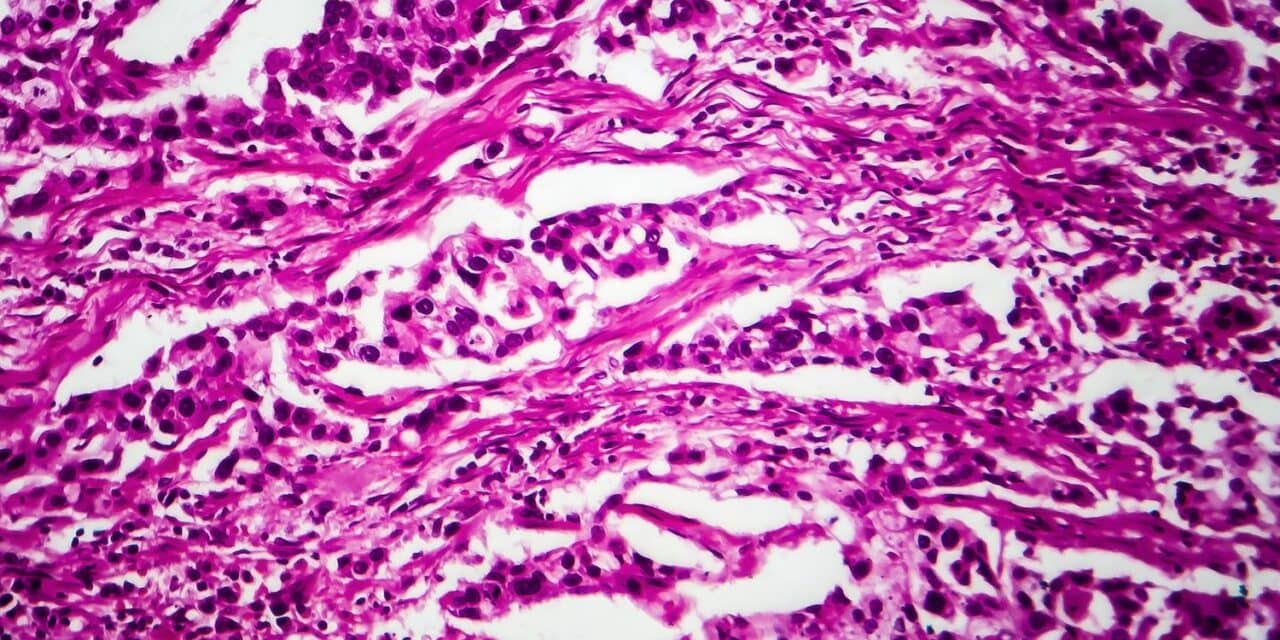
Featured image: Bladder cancer