A new study designed to measure responses to COVID-19 infection found, in some of the sickest patients, a handful of rare structural genetic variants involved in body processes—like inflammation—which the virus needs to be successful.
“The virus has to attach to our cells, it has to get inside our cells and it has to multiply inside our cells. It also has to attract inflammation,” says Ravindra Kolhe, MD, PhD, director of the Georgia Esoteric and Molecular Laboratory at the Medical College of Georgia at Augusta University. “We have identified genes with structural changes in very sick individuals that are part of all four of these essential processes.”
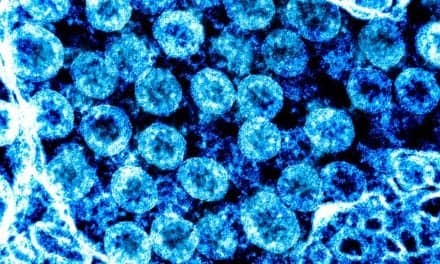
In the study—published by the international collaborative COVID-19 Host Genome Research consortium in the journal iScience—investigators used optical genome mapping to get a thorough, three-dimensional assessment of the genome of 52 severally ill patients with COVID-19.
In nine of the sickest patients, they identified seven rare structural variants affecting a total of 31 genes involved in key pathways mediating the response between a person, or host, and a virus. These include innate immunity, our frontline immune defense against invaders like viruses; the inflammatory response, a key response to an infection that, gone awry, can also destroy the lungs of some of the sickest patients; and the ability of a virus to replicate and spread.
Large structural variants account for much of the genetic diversity among us, including changes that are just unique to the individual and those that can increase their risk of problems like cancer. Optical genome mapping is an emerging technology that can detect these larger variants with multiple changes, like deletion or insertion of genetic material and/or when a section of chromosome is reversed.
The investigators say that while more work needs to be done, their findings about the potential role of structural variants in the host-virus interaction point toward the need to look for genetic variations, ideally with a simple- to-use blood assay. Once identified, the goal would be to initiate proactive moves for these individuals like ensuring vaccination and boosting and potentially more aggressive treatment early on, like monoclonal antibody therapy, to help these individuals better combat COVID, Kolhe says.
Clinical studies have identified factors like older age, being male, hypertension, diabetes and other chronic conditions as risk factors associated with the degree of illness from COVID-19. The nine sickest patients in this study shared common comorbid conditions, 32 of the patients required mechanical ventilation to support their breathing and a total of 13 of the 52 patients died while in intensive care.
But in their studies, which also included individuals who were negative for the COVID-19 virus and those who were positive but asymptomatic, there were again outliers, including individuals with comorbid conditions who remained asymptomatic when infected with SARS-CoV-2 and those who were perfectly healthy but became extremely ill when infected, another indicator of a role for genetics in determining the degree of response, Kolhe says.
Kolhe notes that the large structural variants they found in the sickest patients were not caused by the virus rather used by the virus and may not increase susceptibility to other, even similar, conditions.
Overall, the individuals in this study had about 40 rare structural variants, which other studies have indicated is about average.
Some studies have found that blood type might be a factor in predicting risk, specifically type A, and there have been some specific gene findings as well that predispose to immune deficiencies that may make people more susceptible.
Kolhe, who is also associate director for genomics at the Georgia Cancer Center, has been using optical genome mapping to look for patient-specific cancer-causing variations.
Featured image: Ravindra Kolhe, MD, PhD, director of the Georgia Esoteric and Molecular Laboratory at the Medical College of Georgia at Augusta University. Photo: Michael Holahan, Augusta University