Researchers at Kanazawa University have reported findings that show what causes some lung cancer patients to have an intrinsic resistance to the drug osimertinib: AXL, a protein belonging to the class of receptor tyrosine kinases. The combined application of osimertinib and an AXL inhibitor were shown to limit intrinsic resistance to the drug.
For treating cancer, drugs based on molecules known as tyrosine kinase inhibitors are sometimes used. One such tyrosine kinase inhibitor, osimertinib, has been used to treat epidermal growth factor receptor (EGFR)-mutated lung cancer with a certain degree of efficacy. EGFR is a protein that plays an important role in signaling from the extracellular environment to a cell. However, in some patients, intrinsic resistance and inadequate response to osimertinib has been seen to occur. Seiji Yano, MD, PhD, a professor of medicine at Kanazawa University, and colleagues have discovered that a particular protein known as AXL causes resistance to osimertinib and the emergence of osimertinib-tolerant cells.
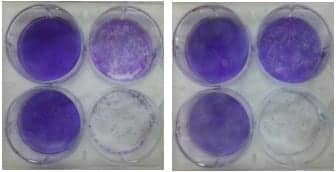
The researchers first showed that, in vitro, osimertinib activated AXL in EGFR-mutated lung cancer cells. Next, they demonstrated an inverse correlation between AXL and susceptibility to tyrosine kinase inhibitors: AXL expression correlated with a poor response to treatment with osimertinib and with early tumor relapse.
Yano and colleagues also checked whether drug-tolerant cells exhibited higher levels of AXL. The tolerant cells were found to display a higher expression of AXL compared to parental cells. Application of an AXL inhibitor called NPS1034 led to a decrease in survival of the drug-tolerant cells.

Outcomes of Kanazawa University research cultures to investigate the origin of resistance to the cancer therapeutic osimertinib. Image courtesy Kanazawa University.
The scientists then investigated the effect of the AXL inhibitor combined with osimertinib in a mouse model. Treatment with only NPS1034 had no effect on the tumors. Treament with only osimertinib initially led to tumor regression, but tumor regrowth was observed within 7 weeks. Simultaneous treatment with NSP1034 and osimertinib led to tumor regression within a week, and the size of the tumors remained stable for 10 weeks. No adverse effects, such as weight loss, were observed during treatment.
The findings of Yano and colleagues provide important insights into the molecular mechanisms causing tolerance to osimertinib in EGFR-mutated lung cancer cells and, particularly, into the role of AXL and the effects of inhibiting its activity. As the scientists note: “These results suggest that treatment during the initial phase with a combination of osimertinib and an AXL inhibitor may prevent the development of intrinsic resistance to osimertinib and the emergence of drug-tolerant cells in EGFR-mutated lung cancer overexpressing AXL.”
AXL regulates various important cellular processes, including proliferation, survival, and motility. In recent years, it has become clear that AXL is a key facilitator of drug tolerance by cancer cells. Yano and colleagues have found that this is also the case for EGFR-mutated lung cancer: a high expression of AXL correlates with resistance to osimertinib, a tyrosine kinase inhibitor, and the emergence of osimertinib-tolerant cells.
For further information, visit Kanazawa University.
Reference
- Taniguchi H, Yamada T, Wang R, et al. AXL confers intrinsic resistance to osimertinib and advances the emergence of tolerant cells. Nature Communications. 2019;10:259; doi: 10.1038/s41467-018-08074-0.
Featured image: Origin of resistance to lung cancer drug discovered. Image courtesy Kanazawa University.