Myriad Genetics Inc, Salt Lake City, has published results from the Individualized Medicine: Pharmacogenetics Assessment and Clinical Treatment (IMPACT) study.1 The study evaluated 1,871 patients with moderate to severe depression who met the overall study criteria, and compared patient outcomes based on the type of ordering physician for patients whose therapy selection was aided by the GeneSight test.
The study found improved outcomes regardless of provider type, but the patients seen by primary care physicians improved the most. Importantly, patients treated by primary care physicians saw 27% greater improvement in depressive symptoms, 35% higher rates of response, and 63% higher rates of remission, when compared to patients treated by psychiatrists.
Major depressive disorder (MDD) is one of the most common mental disorders and can result in severe impairments that interfere with or limit one’s ability to carry out major life activities. MDD is defined as a period of 2 weeks or longer during which there is either depressed mood or loss of interest or pleasure, and at least four other symptoms that reflect a change in functioning, such as problems with sleep, eating, energy, concentration, self-image, or recurrent thoughts of death or suicide. The World Health Organization (WHO) categorizes clinical depression as the world’s leading cause of disability, and the National Institute of Mental Health estimates that more than 16 million adults in the United States had at least one major depressive episode in the past year.2
“The first physicians to typically treat patients with major depression are primary care physicians, so it is critical that they have access to advanced technologies that can help patients as early as possible,” says Bryan M. Dechairo, PhD, executive vice president for clinical development at Myriad Genetics. “The IMPACT study demonstrates that primary care physicians, when aided by the GeneSight test, can achieve excellent patient outcomes that are better than what was seen in the recent GUIDED prospective clinical study.”
Conducted by the Tanenbaum Center for Pharmacogenetics at the UK’s Center for Addiction and Mental Health, the IMPACT study used the laboratory-developed pharmacogenomic GeneSight test to determine specific enzymes and genes related to medication action. The goal is to achieve more-effective therapies by incorporating genetic information.
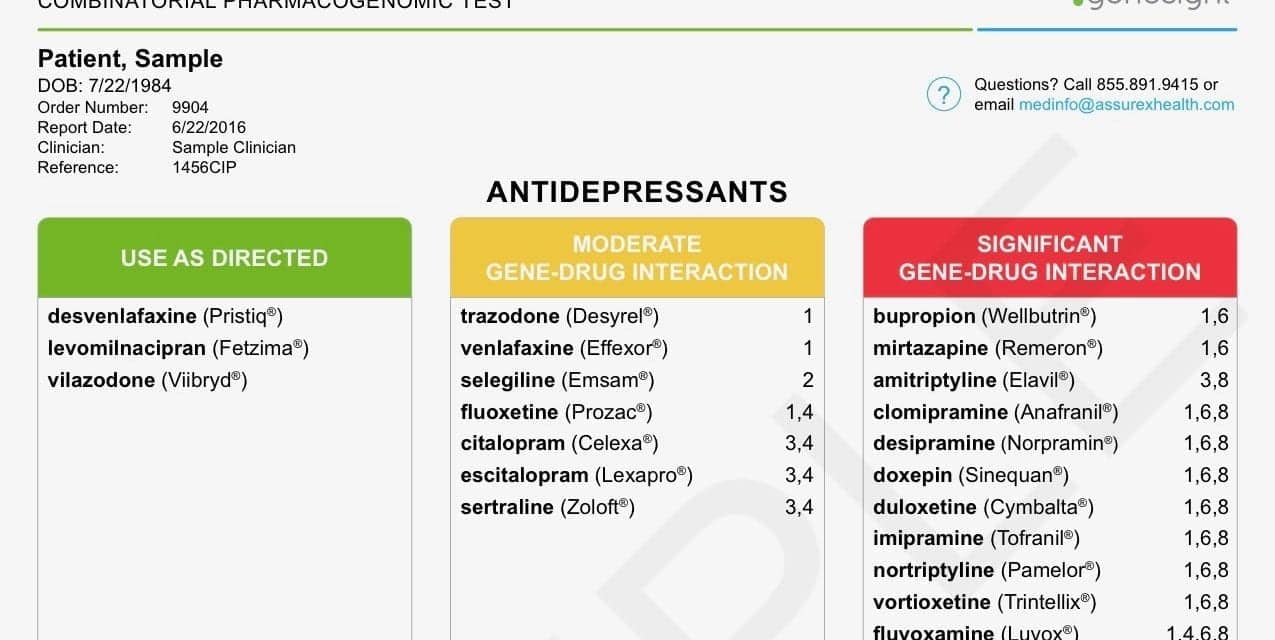
GeneSight uses cutting-edge technology to measure and analyze clinically important genomic variants in the treatment of psychiatric disorders. The results of the GeneSight report can help a clinician understand the way a patient’s unique genomic makeup may influence the effects of certain psychiatric drugs. The analysis is based on pharmacogenomics—the study of genomic factors that influence an individual’s response to drug treatments—manufacturers’ FDA-approved drug labels, peer-reviewed scientific and clinical publications, and proven drug pharmacology. Quick turnaround time, combined with a customized report of the patient’s genomic makeup, clinical experience, and other factors can provide information to help a physician make personalized drug treatment choices for each patient.
To learn more, visit Myriad Genetics.
References
- Tanner JA, Davies PE, Voudouris NC, et al. Combinatorial pharmacogenomics and improved patient outcomes in depression: treatment by primary care physicians or psychiatrists. J Psychiatr Res. 2018;104:157–162; doi: 10.1016/j.psychires.2018.07.012.
- Depression [online]. Bethesda, Md: National Institute of Mental Health, 2018. Available at: www.nimh.nih.gov/health/topics/depression/index.shtml. Accessed August 28, 2018.