TriVerity system demonstrated high sensitivity and specificity across more than 1,200 patients in pivotal SEPSIS-SHIELD trial.
Three studies published in Nature Medicine detail clinical validation results for an AI-powered diagnostic test that distinguishes between bacterial infection, viral infection, and non-infectious inflammation while predicting illness severity in patients with suspected sepsis.
The publications include pivotal results from the SEPSIS-SHIELD study, which evaluated Inflammatix’s TriVerity Test System across more than 1,200 patients. The molecular test uses a panel of 29 patient messenger RNAs to interpret immune response patterns using machine learning algorithms, delivering results in approximately 30 minutes.
“TriVerity radically improves early decisions, telling clinicians whether patients need antibiotics, other diagnostics, or a higher level of care,” says Tim Sweeney, MD, PhD, co-founder and chief executive officer of Inflammatix, in a release. “That clarity can not only drive better outcomes; it also protects hospitals from costly denials.”
The TriVerity system received US Food and Drug Administration (FDA) Breakthrough Device Designation and FDA 510(k) clearance in January 2025. The test is indicated for adult patients with suspected acute infection or sepsis presenting to emergency departments.
Consensus Framework for Immune Dysregulation
A second Nature Medicine paper reports development of the Human Immune Dysregulation Evaluation Framework (HI-DEF), a consensus network created by the SUBSPACE consortium. The framework analyzed transcriptomic data from more than 7,000 patient samples across 37 cohorts worldwide.
HI-DEF measures dysregulation in myeloid cells and lymphoid cells, classifying patients into four states: balanced, myeloid-dysregulated, lymphoid-dysregulated, or system-wide dysregulated. Patients with myeloid or lymphoid dysregulation were 5-7 times more likely to die or require intensive care unit-level care, with highest mortality among those with system-wide dysregulation.
“Identification of virtually identical conserved endotypes across critical illnesses by two international consortiums upends decades of failed research in sepsis, and in critical illnesses more broadly, due to biological and clinical heterogeneity in patients,” says Purvesh Khatri, PhD, professor of medicine at the Stanford School of Medicine and co-corresponding author, in a release.
Analysis of multiple randomized control trials using HI-DEF scores found associations with differential mortality in patients treated with immunomodulatory drugs such as anakinra and corticosteroids.
Blood Transcriptomic Subtypes Identified
The third Nature Medicine paper describes identification of three consensus transcriptomic subtypes of sepsis based on analysis of 2,142 blood samples from patients across four cohorts. The subtypes, referred to as CTS1, CTS2, and CTS3, showed varying mortality rates, with CTS2 demonstrating the highest ICU mortality at 28.6% compared to 16% in CTS1 and CTS3.
The CTS clusters facilitated identification of patients who may or may not respond to steroid treatment. The three CTS endotypes corresponded to three of the four HI-DEF endotypes.
“We are implementing TriVerity in our ER,” says Edward A. Panacek, MD, professor and chair of emergency medicine at the University of South Alabama, in a release. “We have never had a tool that can both improve patient care and reduce costs — until now.”
The TriVerity Test System includes the proprietary TriVerity cartridge and the Myrna instrument. Development was supported in part by funding from the US Department of Health and Human Services Biomedical Advanced Research and Development Authority under multiple contracts.
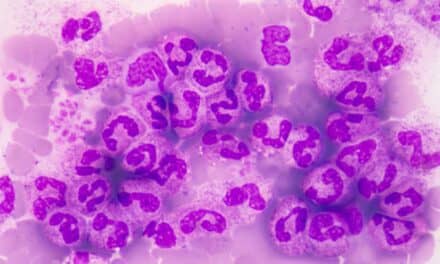
Photo caption: TriVerity
File Photo/Inflammatix