Labs address personnel shortages, expanding functions, new technologies, and the need for standardization
By Gary Tufel
Laboratories and laboratorians in the histotechnology sector are facing a variety of ongoing challenges. Among the most commonly cited issues are the shortage of qualified histotechnologists and the increasing influx of more sophisticated specimen testing—followed closely by a need for the standardization of testing processes and results. Of necessity, these pressing issues are being addressed, but how, to what extent, and with what level of effectiveness?
According to Michael Nalesnik, MD, professor of pathology in the division of transplantation pathology at the University of Pittsburgh Medical Center, today’s histotechnology lab is caught among the pressures of several external forces. Labs must deal with issues of decreasing reimbursement, declining availability of trained personnel (see the sidebar, “Meeting the Ongoing Histotech Shortage”), and a rapid increase in such technological advances as molecular and genetic testing, automation, and computerization—all of which are placing more demands on labs.
“To meet these demands, labs are being forced to shift from being classical histology labs to becoming more like diagnostic histotechnology centers,” says Nalesnik. “Today’s labs must be able to anticipate the effects of contrasting changes in the medical environment, such as a larger aging population, which may increase volume; and greater use of less-invasive or point-of-care testing, which may reduce lab volume.”
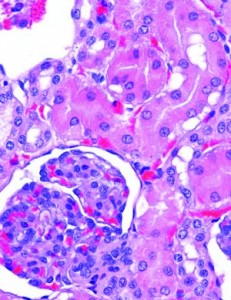
In addition, Nalesnik notes a likely shift in the types of test specimens processed and a demand for more information from each test. Assays such as estrogen, progesterone, or HER2/neu tissue testing will, in retrospect, be seen as the tip of the iceberg, as additional markers with diagnostic and therapeutic implications for a bewildering variety of diseases are developed and find their way into clinical practice.
With such increasing complexity, the need for standardization overseen by appropriate regulation is inevitable. “The changes are challenges, but they’re not negatives,” says Nalesnik. “Labs are there to serve patients by providing pathologists with the proper material to help them diagnose disease and, in some cases, to suggest more effective therapies. The changes are a crucial part of 21st-century pathology practice. But everything starts with histotechnology and is amplified from there.”
STANDARDIZATION AND AUTOMATION
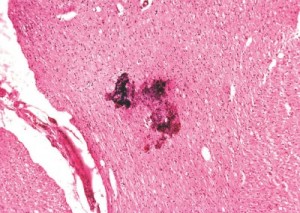
Avoiding errors in testing is yet another challenge in the histotechnology lab. Transcription errors and tissue “floaters,” which can be created using the traditional “dip and dunk” slide sample testing method, are two examples of errors that can lead to misidentification of patient samples. Nalesnik says some studies show that about 1% of all surgical pathology cases have some form of error. Of those, about 6% can potentially lead to patient harm.
[reference float=”right”]Preanalytics and Imaging for Histology
Many companies provide products and services to labs for histology testing. For histology labs, adopting new technologies in preanalytic processing, digital pathology and whole-slide imaging, and image analysis can create significant challenges. Fortunately, a number of firms are active suppliers in these areas, helping to guide labs through current and advancing technologies.
Following is a list of some of the major firms in the preanalytics and imaging subspecialties of histotechnology. For additional listings, visit the CLP Buyer’s Guide, under the main category heading “Cytology/Histology/ Histotechnology.” There you’ll also find additional subcategories and lists of companies active in those specific areas.
- Definiens
www.definiens.com
- ELITech Biomedical Systems
www.elitechgroup.com - Hamamatsu
www.hamamatsu.com - Leica Biosystems
www.leicabiosystems.com - Mikroscan Technologies Inc
www.mikroscan.com - Milestone Srl
www.milestonemedsrl.com - NovoPath
www.novopath.com - PerkinElmer
www.perkinelmer.com - Philips Digital Pathology
www.research.philips.com/
initiatives/digitalpathology - Sakura Finetek USA Inc
www.sakura-americas.com - 3DHisTech
www.3dhistech.com - ViewsIQ
www.viewsiq.com[/reference]
Concern for the impact of such errors underscores the significant need for standardization in the histotechnology lab. “If we keep doing these things the same way, the problem will persist,” says Nalesnik. “However, the solution is not to push techs to work harder—they are already working at maximum capacity—but to provide additional help through the introduction of automation. Chemistry labs led the way years ago. Histotech labs, which have a much more complicated workflow, are now following suit.”
“Labs are at a crossroads,” says Nalesnik. “They can remain as they were. Or they can cope with the new complexity. That’s where training comes in. Since everything in the testing process starts with histotechnology, any problems here will be amplified downstream when applying newer technologies.”
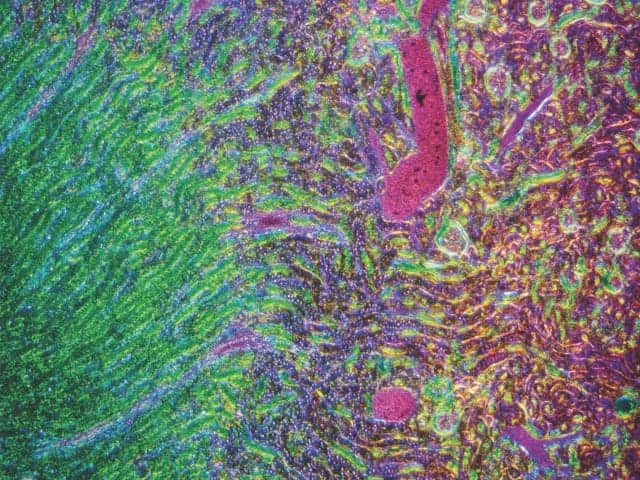
Nalesnik cites digital pathology slide imaging and analysis, a new technology now in various phases of adoption in labs, as an example of the challenges. Not only do labs need to find physical space for the new machines, but quality control has to be more stringent in order to keep samples pristine and free of folds, dust, fingerprints, and other flaws that can make the entire imaging process fail.
The challenge for labs is to incorporate these new technologies appropriately. If individual labs do not remain integral to the process, they risk becoming irrelevant. There’s also a big financial risk, especially with reimbursement rates decreasing. Molecular testing and other new technologies, such as nanotechnology using quantum dots, will continue to evolve and present labs with similar challenges, says Nalesnik.
And labs must keep up and continue to add value to biopsies, Nalesnik notes. Digital monitors will eventually replace the microscope, and labs will also be asked to provide such information as what genes are involved and what drug treatments to use. The technology may even fragment into different disciplines. “So labs have to stay relevant,” he says.
Beth Sheppard, MBA, HT(ASCP), senior director for market access at Ventana Medical Systems Inc, Tucson, Ariz, agrees that histology labs’ many challenges include reduced reimbursement rates and skilled staff shortages, and she adds that there is also pressure to reduce turnaround time. All of this leads to increased stress on the staff, which in turn can lead to greater potential for errors.
To relieve such pressures, an increasing number of labs are implementing higher levels of automation, as part of a Lean workflow process designed to increase capacity and standardize operations. Throughout the anatomical pathology processes of many labs, for example, there has been wider implementation of barcode specimen tracking systems. Such systems help to reduce labeling errors, provide specimen accountability, and monitor turnaround time.
Patient safety is of paramount importance, says Sheppard, so it is important that labs reduce the potential for patient sample cross-contamination in all histology processes, including hematoxylin and eosin staining. As a result, automated systems and process controls created for this purpose are gaining more attention in the lab.
However, there are currently no standardized methods for handling and documenting errors that occur in histopathology labs, so the need for consensus recommendations and guidelines in this area is gaining traction. There is also an emphasis on standardizing technical best practices—especially for the preanalytic phase, where the quality and accuracy of staining have the greatest implications for the patient’s diagnostic outcome. “There is definitely an increasing emphasis on how the pathology community can continue to improve patient safety,” Sheppard says.
Similar to the evolution that occurred for clinical chemistry labs in the past, histology labs are now striving for broader adoption of automation. The use of automated systems will enable histotechnologists to move into other advanced tissue-based diagnostics and digital pathology. But in turn, such a new approach will require that histology professionals remain competent through continuing education, and therefore continue to be recognized as the custodians and subject matter experts when it comes to patient tissue samples.
As one example, Craig Pow, director of business development and international marketing at Vector Laboratories, Burlingame, Calif, says his company is familiar with standardization in the immunohistochemistry (IHC) area, and supports the standardization of lab techniques from the point of view of the reproducibility and validity of results. “The number of variables involved with laboratory techniques—and those left to the discretion of the end user—can certainly contribute to a lack of reproducibility or less than satisfactory results. In turn, this could directly affect interpretation of the stained tissue sections,” Pow says.
“Avoiding false positive and false negative results is paramount for achieving reliable IHC results in both research and clinical settings,” Pow adds. “The key step for overcoming these issues should be the establishment of set parameters for crucial tasks such as tissue preparation.”
As the current president of the National Society for Histotechnology, Sheppard has a feel for the trends that are influencing the development of the field. In the future, she says, histotechnology will extend into molecular diagnostics and PCR, and advanced histological techniques will be vital to personalized medicine and companion diagnostics.
In the meantime, some innovations, such as barcoding, are already reducing the number of human errors in the lab, says Nalesnik, and if implemented correctly, they remove the tedium associated with repetitive tasks. “Automation is best used to streamline the workflow and support the techs. It cannot replace them.”
HISTOLOGY LABS’ EXPANDING FUNCTIONS
In keeping with Sheppard’s observations, it is clear that the practice of histology is expanding to include various forms of companion diagnostic tests to accompany cancer treatment choices, and molecular and other testing technologies that help characterize tumors. Right now, the entire field is very dynamic and exciting, says John D. Allen, MBA, MT(ASCP), director of laboratory services at Tucson Medical Center. “I anticipate that healthcare payors will want to invest in much more testing of tumors and other tissues to help make very important decisions that can facilitate exceptional savings downstream in the healthcare continuum.
“The trend is to differentiate cancerous tumors by their metabolic mutations in order to guide focused therapy, instead of just determining the organ of origin,” Allen says. “These two concepts could shift the paradigm in treatment decisions, and could ‘bend the curve’ toward reducing healthcare costs, by making targeted cancer therapy much more successful. In turn, the healthcare system would avoid the considerable costs caused by missteps in the treatment process.”
[reference float=”right”]Diversified Histology
Some firms produce testing products in several subspecialties relating to histology. For more information, visit the CLP Buyer’s Guide, under the main category heading “Cytology/Histology/ Histotechnology.” The companies below appear in a number of subcategories.
- Philips
www.usa.philips.com/
healthcare - Thermo Scientific
www.thermoscientific.com - Ventana Medical Systems Inc
www.ventana.com[/reference]
But in order to become the logical personnel to perform such testing, histotechnologists will have to learn new skills, says Allen. And at the same time, advanced diagnostics that are now available only from specialty laboratories will need to be performed much closer to the patient—even right in the hospital lab where routine histology is performed.
“There will likely be opportunities to regionalize this kind of testing, bringing the testing process closer to the patient, and making the results available to surgeons and oncologists more quickly,” says Allen. “Much of this testing is being developed using more accessible staining techniques that could make them practicable to mainstream histology departments.”
And because much of this testing involves the use of new technologies, it will be important that laboratories excel in using their informatics and pathology experts to provide clear, succinct interpretations and guidance to the clinicians who are taking care of patients. Histology labs are the repositories of large amounts of clinical data, but getting the most value from its potential will require laboratorians to provide sound interpretations and guidance to therapy choices based on some of the newest and most complex types of genomic testing.
“We in the laboratory space must address the challenges of converting our new-age data into usable information for clinicians,” says Allen. “In that way, we will solidify the value of laboratory services—including histotechnology and molecular technology.”
This is a very exciting time for histotechnology and its associated testing, concludes Allen. Labs and laboratorians who are ready to take on the challenges will surely be rewarded by knowing that they are contributing to significantly improving the odds of conquering cancer, patient by patient.
For more information, visit the companion article, “Meeting the Ongoing Histotech Shortage.”
Gary Tufel is a contributing writer for CLP. For further information, contact chief editor Steve Halasey via [email protected].