|
|||
| Dave Hickey, Siemens | Fred V. Plapp, St. Luke’s Health System | Mary Steele Williams, Association for Molecular Pathology | Brian Jackson, ARUP Laboratories |
Midyear 2007 brings a new look at trends and challenges. Which innovations do industry professionals expect in various areas of clinical lab practice – particularly in products? And what do they see in the future?
The CLP Industry Roundtable was conducted via telephone and e-mail.
Participants were:
- Dave Hickey, VP, Siemens Medical Solutions Diagnostics, Strategic Marketing & Planning
- Fred V. Plapp, MD, PhD, laboratory medical director, St. Luke’s Health System
- Mary Steele Williams, MT, SM, COO, director of scientific programs, Association for Molecular Pathology
- Brian Jackson, MD, MS, medical director of informatics, ARUP Laboratories, and assistant professor of pathology, University of Utah
What is your opinion on trends in the area of point of care?
Hickey: This is an area of future growth and I believe there will be a demand for more products in this area. In deciding which products are truly needed, we should ask ourselves whether having a quick turnaround time for the result will make a real difference in clinical intervention at the bedside. Will the doctor do anything different?
POC vendors should truly understand the needs of their customers as they relate to the types of tests and technology that would provide a clinical benefit if utilized at the point of care.
IMAGING, INFORMATICS, AND
IN VITRO DIAGNOSTICS
Siemens recently acquired Bayer Diagnostics and Diagnostic Products Corp. How will this affect the clinical lab industry?
Hickey: The acquisitions were an integral part of delivering on Siemens’ vision and strategy. Defining health care today requires a new way to look at the health care continuum model of prevention, diagnosis, treatment, and ongoing care. The cost burden and inefficiencies prevalent in the current systems are because we tend to diagnose and treat once disease is present, and often at a chronic stage.
The question is: How can we improve overall health care delivery while reducing costs? Early disease detection, disease prevention and screening are, we believe, a significant part of the answer. With that model in mind, Siemens’ vision is to build a solutions portfolio that can facilitate the delivery of efficient health care all along the health care continuum.
With the acquisition of Bayer and DPC into Siemens Medical Solutions, we are now capable of delivering a fully integrated diagnostic model—in vivo, in vitro, and clinical informatics working as one.
Siemens is a strong player in the POC arena today, and particularly in the areas of blood gas, urinalysis, and diabetes (HbA1c testing). In other areas of POC we see growth in oncology, infectious disease, and cardiac testing. Cardiology products, for instance, are an area of high interest in the POC community, and newer equipment is being developed to better and more quickly diagnose such things as acute cardiac infarctions.
Plapp: Point-of-care testing continues to grow at a rapid rate in order to meet turnaround time expectations of nurses and physicians.
Glucose meters continue to comprise the highest volume of point-of-care testing. The introduction of tight glycemic control protocols in hospitals has increased the need for more accurate bedside glucose meters.
In 1987, the American Diabetes Association (ADA) recommended that glucose meters should have a total error (analytic plus user) of < 10% at glucose concentrations between 30 to 400 mg/dL. More recently, ADA urged manufacturers to further decrease total error to 5%. Currently available meters do not meet these performance goals. Recent proficiency testing results from the College of American Pathologists demonstrate that glucose meters have much more instrument-to-instrument variability than chemistry analyzers in central laboratories. For example, the interlaboratory precision at a glucose value of 400 mg/dL ranged from 4.1% to 13.7% for glucose meters compared to 1.6% to 2.8% for chemistry analyzers. In order to decrease glucose meter variability, instruments of the future need to incorporate upgrades that reduce the opportunity for operator error as much as possible. Blood volume requirements need to be reduced to eliminate errors due to underfilling of strips. Glucose meters should not report a result if the strip is either under- or overfilled. Analytical time should be reduced to less than 10 seconds. The adverse effects of hematocrit and interfering substances, such as maltose, need to be eliminated. Software enhancements are needed to validate operator entry of patient identifiers.
The proliferation of different types of point-of-care testing, in addition to glucose meters, has created a regulatory and compliance quagmire for laboratories and hospitals. All future point-of-care instruments need to incorporate built-in quality control and operator identification lockouts to improve compliance.
The placement of so many point-of-care devices throughout the hospital and outpatient clinics has emphasized the increasing need for wireless connectivity and improved data management systems to ensure that results are entered into the EMR in a timely fashion.
Jackson: As medical director for Informatics at ARUP, I pay less attention to chemistry and physiology than I do to care processes and information flow. In that respect, I think the biggest POC opportunities are in helping care processes move from high-expense medical settings to lower-expense settings, as well as in reducing the need for follow-up visits. Handheld glucometers and over-the-counter pregnancy tests have been successful because they have allowed care processes that used to take place in hospitals and clinics to move into the home.
Other POC tests, on the other hand, simply take tests that work just fine in the clinical laboratory and replace them with faster versions that are often more expensive and less accurate. For example, the American Gastroenterological Association recommends use of either stool antigen or breath test (not serology) for diagnosis of Helicobacter pylori infection. POC H pylori IgG testing is becoming popular at some hospitals and clinics, however, even though it doesn’t do anything to shift care toward a less expensive setting. Plus, the poor specificity may lead to overdiagnosis and overtreatment.
If I were a POC vendor, I would look for care processes that could be made much more efficient and less expensive, if only a particular lab test could be moved to the point of care. I would also limit my attention to tests for which speed and availability are the only current clinical limitations, not test accuracy.
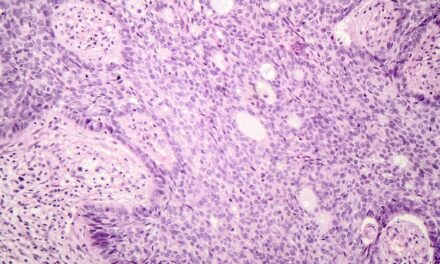
What are the trends and challenges in anatomic pathology?
Hickey: Like the central laboratory, the technology and equipment in this area is advancing and becoming increasingly digitized. Anatomic pathology departments are moving more towards automation in order to improve workflow and specimen turnaround times. Tissue testing and anatomic pathology will play an important role in the model of personalized medicine, where a more preventive approach is being taken. There’s more screening done and more will be done than is today, when treatment comes later. Gene expression and gene profiling will enable doctors to look at genetic makeup in tissues and cells, allowing earlier diagnoses and treatment than is currently possible.
Jackson: In the AP space I’m interested in integration of information, particularly genetic and other novel markers, into the final diagnosis. Although there have been impressive efforts by the College of American Pathologists and others to standardize certain diagnostic algorithms, such as Her2/neu in breast cancer, much of anatomic pathology diagnosis remains qualitative and/or subjective. In that environment, new markers have the potential to confuse clinicians rather than assist them. I have seen interesting work by both academic and boutique AP labs to present multiple related test results on a single graphical integrated report, which is a step in the right direction. The next steps will include linking these reports to likelihood ratios and summaries of the supporting evidence for the applicable markers.
What are the significant developments in molecular diagnostics/genetic testing?
Hickey: This is a huge growth area that is still evolving. Testing has traditionally been thought of at a bacterial and viral level in such areas as hepatitis and HIV, but today it’s evolving into other disease states such as oncology and cardiology—areas where molecular diagnostics can be applied.
Gene expression and gene profiles offer better prognoses because through genetic testing we are able to detect disease much earlier. Methods in use today are mostly in a research environment, but they will become part of routine clinical diagnostics as we move forward.
Plapp: Although molecular testing has been available for many years, automation is just now being introduced. The Cepheid GeneXpert is the first fully automated FDA-cleared instrument platform that does DNA preparation and real time PCR analysis. Roche’s Cobas Ampliprep/Cobas TaqMan system for HIV testing is also a fully automated, FDA-cleared system for HIV viral load testing. The introduction of these fully automated platforms will make it possible for more labs to implement molecular testing because dedicated molecular laboratory space will no longer be required.
The GeneXpert Group B Streptococcus assay is FDA-cleared as moderate complexity, which is the first time a molecular test has been classified as such. This automated instrument may even be placed in an automated or rapid-response laboratory instead of in a molecular laboratory to facilitate 24/7 testing. A perfect example of this application is stat enterovirus testing for patients admitted to the emergency department with suspected meningitis. Patients who test positive can be discharged, while patients who test negative can be admitted and treated with antibiotics for possible bacterial meningitis.
Medical practice for diagnosing group A streptococcus is changing. Some experts recommend replacing rapid strep tests in physician offices with a molecular assay, because of its higher sensitivity. Alternatively, group A strep PCR testing can replace culture as a more rapid confirmatory test for patients with negative rapid strep tests.
Traditional virology laboratory procedures will gradually be replaced by molecular testing. Molecular testing is now considered to be the gold standard for two of the most commons viruses—herpes simplex virus and cytomegalovirus. In the near future, molecular testing will be performed for the rapid diagnosis of respiratory illnesses.
Molecular tests are being implemented to screen for and monitor hospital-acquired infections such as methicillin-resistant staphylococcus aureus and vancomycin-resistant enterococcus. More hospitals will initiate these screening programs to decrease the risk of nosocomial infections.
Pharmacogenomic testing will become reality in the very near future. Warfarin is being relabeled to include a recommendation for genetic testing. The advent of this high-volume testing may open up other opportunities as physicians embrace the concept of pretreatment pharmacogenomic testing. Molecular tests are being used more frequently to classify leukemia and lymphoma and to assess remission status. Studies are ongoing that may further indicate a prognostic role for many of these tests.
The laboratory is experiencing a rapid increase in the number of esoteric tests, including molecular diagnostics. Physicians are having difficulty staying abreast of this information explosion. Pathologists and laboratories will need to provide more meaningful interpretive reports to assist physicians in understanding the clinical significance of these tests. Comprehensive Web sites, such as www.clinlabnavigator.com and www.arupconsult.com, will play an increasingly important role in physician education.
Laboratory information systems (LIS) and electronic medical records (EMR) have not kept pace with the rapid expansion of molecular diagnostics. Only Cerner Corp and SCC Soft Computer have developed LIS modules specifically for molecular diagnostic laboratories. The major obstacles to effectively communicating molecular testing results to the EMR is the lack of standard nomenclature for molecular methods and genes and their mutations, and the inability to easily translate complex molecular data into a meaningful interpretive clinical report. Because much of the more esoteric molecular testing will be performed in reference laboratories, common standards will be needed to permit transmission of this data to hospital LISs and EMR. Future EMR will need to graphically display the data.
Williams: Molecular diagnostics has emerged fully from research into clinical practice. Instrumentation now automates many of the sample preparation and assay steps that were formerly labor intensive. New tests are being launched all the time. Many molecular tests are FDA-cleared or -approved, and more are in the pipeline. Because molecular testing is indicated in so many areas of health care—cardiology, oncology, infectious diseases, inherited diseases and disorders, just to give you a sampling—laboratory directors should be familiar with the tests available and their applications.
The metabolism of many drugs is affected by our genetics; therefore, pharmacogenetic testing is essential to appropriate patient care, and it appears on the labeling of a number of drugs. For these reasons and more, labs need to be prepared to offer molecular testing at least as a send-out, even if they are not in a position to offer the tests in-house.
AMP has resources to help laboratory professionals understand and adopt molecular testing. We are offering an outreach course in Los Angeles on November 7 for laboratory professionals who have little or no experience in molecular diagnostics. The course is held the day before our annual meeting. Those who attend the course get a free pass to visit the exhibit hall, where they can interact with approximately 100 manufacturers of molecular tests. Our Web site, www.amp.org, has a listing of FDA-cleared/-approved molecular tests accessible from the home page. We also have an online test directory, www.amptestdirectory.org, which lists the tests offered by the laboratories of AMP members. It is a terrific resource for clinicians, laboratories, and the public.
When I was a kid watching “Star Trek,” I was fascinated by the possibility of medicine as practiced by Dr McCoy. I hear that there are similar technologies closer to being available than we might think. Microarrays, nanotechnology, and molecular imaging are already in use. Who knows, perhaps tomorrow we will see tricorders!
Jackson: As more and more sequencing is performed in clinical laboratories, a critical emerging issue is how to handle uncertain variants, ie, variations from the reference sequence that have not been definitively determined in the literature to be either disease-causing mutations or benign polymorphisms. Several approaches include family studies, sequence conservation across species, and protein structure prediction. Laboratories performing full-gene sequencing will be under increasing pressure to provide this level of analysis, rather than simply reporting “variant of uncertain significance identified.”
What about automation?
Hickey: The central laboratory is using equipment and solutions that bring a significant degree of automation. This allows staff to migrate to more specific testing areas.
Labs generate a lot of work and data, interpreting, handling and distributing large volumes of results and information to physicians.
Each lab wants to increase its own competitiveness and the repertoire of tests it can do. The barrier has been the lack of adequate levels of staffing and skills. But automation can handle routine lab work, thus freeing up staff for more skilled tasks.
Plapp: Laboratories will increasingly adopt automation in the future to reduce errors and improve efficiency. Total laboratory automation systems are too large, complex and expensive for many smaller hospital or private laboratories. Workstation-based systems, comprised of a specimen sorter connected to several analyzers, will be more appealing to these laboratories.
Laboratories offering outreach services are less able to standardize the size of tubes that clients send to the laboratory. Automation systems of the future should accommodate different tube sizes.
Preanalytical labor and error rates will be significantly decreased by bar coding specimens at the bedside and automating accessioning.
Efforts to reduce the volume of blood drawn from patients have resulted in an increase in the number of tests being ordered on specimens already received in lab. Postanalytical automation will significantly improve laboratory efficiency by automating specimen storage and retrieval.
Newer automation systems should be flexible enough to allow laboratories to attach different manufacturers’ instruments with their automated systems. This flexibility will allow laboratories to automate without replacing all of their existing analyzers.
Williams: Automation brought about a major change in laboratory testing, and molecular testing is no exception. The footprint of instrumentation has become smaller so it is easier to bring tests on board. Random access capability offers flexibility.
A number of companies offer FDA-cleared and approved molecular tests and ASRs for laboratory developed molecular assays. Roche (AmpliChip) and Autogenomics (Infiniti) are two examples of companies that manufacture tests for Cytochrome P450 genotyping. Cephied’s GeneXpert is notable in that it performs tests that are classified as moderate complexity, making it available to the general CLIA-certified laboratory. The GeneXpert performs tests for Group B strep and MRSA, as well as others; therefore, it is very useful to have these tests available 24/7.
It is important to note that even though performance of the assays themselves has become easier, the interpretation of many tests is still complex and is best left to professionals who have a thorough understanding of the workings of complex genetics. The good news is that an increasing number of schools have programs to train molecular laboratory professionals.
Automation enhances laboratory testing; it does not threaten jobs. Laboratories are near crisis regarding technical staffing in general, but particularly when it comes to molecular testing. I don’t believe that automation has anything to do with this. Fewer people are choosing medical technology as a career, and more people are leaving to pursue better opportunities. I also understand that a wave of retirements is expected to decimate lab staffs very soon. Decreased production and increased destruction means that the laboratory, and concomitantly, patient care, can become anemic. Administrators who are forward-thinkers regarding testing technology and capacity-builders regarding staffing are going to be the big winners. Patients who have access to testing by such laboratories are fortunate indeed.
Jackson: While specimen-handling automation/robotics continues to be an interesting area, I see the biggest automation opportunities on the information-handling side. Instrument-LIS interfaces and autoverification continue to be big weaknesses, particularly with smaller platforms and vendors who are new to the clinical laboratory market. These technologies can provide modest clerical labor savings, but I would expect that the reductions in tedious data review and data entry would more than make up for perceived threats to job security, particularly given the current technologist shortage.
Gary Tufel is a contributing writer to CLP.