Summary: Hardy Diagnostics released a new Auris Enrichment Broth to detect and identify Candida auris from skin samples.
Takeaways:
- Candida auris is a serious multi-drug resistant fungal pathogen that can persistently colonize the skin and hospital environments, making it difficult to control in healthcare settings.
- Hardy Diagnostics’ new Auris Enrichment Broth includes chloramphenicol and gentamicin to select against unwanted bacterial growth and is recommended by the CDC for surveillance of C. auris.
- Environmental persistence of C. auris necessitates stringent disinfection procedures in healthcare settings to prevent transmission, highlighting the importance of routine cleaning and the use of fungicidal disinfectants.
Hardy Diagnostics announced its latest product release in the battle to detect and identify Candida auris from skin and environmental samples. The medium is based on the Centers for Disease Control (CDC) formulation for Sabouraud Salt Dulcitol (SSD) Broth with chloramphenicol and gentamicin.
About Candida auris
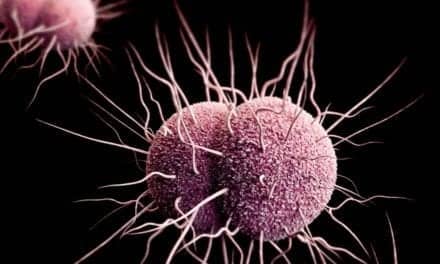
Candida auris is an evolving fungal healthcare-associated pathogen that represents a serious multi-drug resistant (MDR) global threat. Though the organism often presents fewer virulence factors than Candida albicans, C. auris may persistently colonize the skin and hospital environment, making its transmission within and between healthcare settings more difficult to control¹,².
C. auris fungemia results in a wide range of mortality rates (from 32%-66%), depending upon the patient’s overall condition, underlying disease, geographic region, access to medical care, and age³. A review of the organism’s genome demonstrates it harbors genes well-characterized as virulence factors in other Candida species, as well as genes for biofilm production and MDR transcription factors³.
Auris Enrichment Broth
Hardy Diagnostics’ Auris Enrichment Broth is based on the CDC formulation for Sabouraud Salt Dulcitol (SSD) Broth with Chloramphenicol and Gentamicin, as outlined by Welsh et al.⁴. The medium, sometimes referred to as Salt SAB Broth, maintains a lower pH to encourage the growth of fungal isolates. The broth contains dulcitol as the sole carbon source, and chloramphenicol and gentamicin as selective agents against unwanted bacterial growth. Peptones provide nitrogen and amino acids.
The CDC protocol recommends this broth for surveillance of C. auris from skin swabs and environmental samples⁵. Positive broth samples may be subcultured to chromogenic media, such as HardyCHROM Candida + auris (Cat. no. G343), for further identification. Suspect colonies with a teal-to-teal-green “bullseye” center will fluoresce on this chromogenic medium and can be confirmed on the MALDI-TOF.
Environmental Persistence and Disinfection
C. auris may persist on environmental surfaces in healthcare settings and has been cultured from multiple locations in patient rooms. The organism exhibits some degree of tolerance to disinfectants, allowing it to survive on surfaces for greater than three weeks⁶. It can be found on high-touch surfaces near the patient’s bedside, such as tables, rails, and carts; mobile or reusable equipment shared between patients such as blood pressure cuffs, glucometers, temperature probes, and ultrasound machines; and even on surfaces further away from the bedside such as windowsills⁵.
Further reading: Hardy Diagnostics Releases Group A Strep Agar
Environmental disinfection procedures should include routine cleaning and disinfection of patient rooms, as well as mobile and reusable equipment. Fungicidal disinfectants should be used following the manufacturer’s directions. Environmental sampling may be useful in instances of outbreak investigations, surveillance, or to determine the reservoirs of ongoing transmission.
References:
- Anderson, N.L., et al. Cumitech 3B; Quality Systems in the Clinical Microbiology Laboratory, Coordinating ed., A.S. Weissfeld. American Society for Microbiology, Washington, D.C.
- Isenberg, H.D. Clinical Microbiology Procedures Handbook, Vol. I, II & III. American Society for Microbiology, Washington, D.C.
- Rossato, L. and A.L. Colombo. 2018. Candida auris: What Have We Learned About its Mechanisms of Pathogenicity? Frontiers in Micro.
- Welsh RM, Bentz ML, Shams A, Houston H, Lyons A, Rose LJ, Litvintseva AP. 2017. Survival, persistence, and isolation of the emerging multi-drug resistant pathogenic yeast Candida auris on a plastic healthcare surface. J Clin Microbiol 55:2996–3005.
- The Centers for Disease Control and Prevention (CDC). Screening for Candida auris colonization in healthcare settings: CDC Screening
- Dire O., A. Ahmad, S. Duze, M. Patel. Survival of Candida auris on environmental surface materials and low-level resistance to disinfectant. 2023. J. Hosp. Infect. 137:17-23.