University of Washington researchers find rapid test could improve treatment rates but may face implementation barriers due to reimbursement challenges.
A new rapid hepatitis C test that provides results within an hour could help identify more patients for life-saving treatment, but high costs may limit its adoption unless insurance reimbursement increases, according to researchers from the University of Washington School of Medicine.
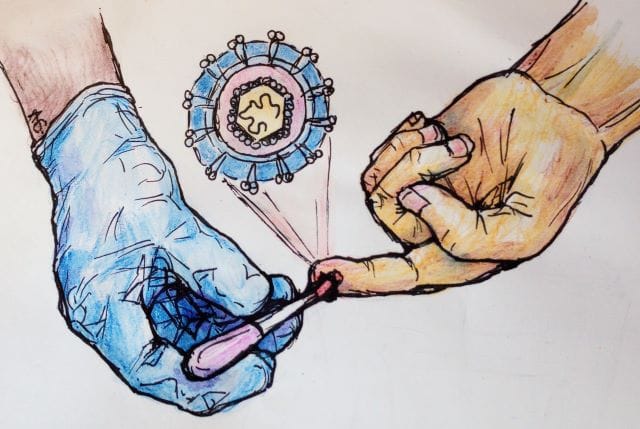
The recently approved Cepheid Xpert HCV test detects the presence of the virus’ RNA through a simple finger-stick procedure and can be performed in doctors’ offices, clinics, or emergency rooms. Unlike traditional hepatitis C tests that can be run in large batches, the new point-of-care test must be run individually and costs approximately $91 per test.
“Our clinicians say that if they were able to go…with these lab results for these patients while they are still in the ER or clinic, they would be able to convince them to start treatment right on the spot,” says Alexander Greninger, MD, PhD, professor of laboratory medicine and pathology at the UW School of Medicine and senior author of the study, in a release.
Rising Infection Rates Drive Need for Better Testing
The Centers for Disease Control and Prevention estimates that as many as 4 million Americans have chronic hepatitis C, with about 70% of infected individuals developing chronic infections that can cause cirrhosis, liver failure, and cancer. Most patients are unaware they are infected due to lack of symptoms.
While early screening efforts successfully identified older Americans with high infection rates, recent years have seen rising acute and chronic infection rates among younger adults, largely due to the opioid and injection drug-use epidemic. These patients, often seen in community clinics and emergency rooms, frequently do not receive treatment.
Available treatments clear hepatitis C infection in about 90% of patients, making early detection and immediate treatment initiation critical for successful outcomes.
Cost Analysis Reveals Implementation Challenges
To assess implementation costs, Greninger and colleagues analyzed hepatitis C testing across the UW Medicine healthcare system from 2017 to 2024. The system includes a major medical center, a public county hospital, a community hospital, and primary- and specialty-care clinics around King County.
“Even a minimal implementation of this test, such as restricting it to orders from the county hospital emergency room, would increase overall HCV testing lab costs by 22%, while broader implementation would cost millions of dollars, at a time of declining test reimbursements and challenging budgets throughout health care,” says Dr Emily Helm, a UW resident in laboratory medicine and pathology and lead author of the study, in a release.
Strategic Implementation Could Improve Cost-Effectiveness
The researchers found that restricting test use to high-risk patient settings would be most cost-efficient. At Harborview Medical Center’s emergency department, where more than 10% of hepatitis C tests were positive, limiting the new test to this location would increase lab costs by about $550 per infection detected.
About one-third of King County hepatitis C cases are diagnosed in Harborview’s emergency department. Testing hospitalized patients at the public county hospital was also relatively cost-efficient compared to other approaches.
Greninger says that eradicating HCV “is about finding cases—the diagnostics—and the challenge is to find new ways to implement these tests that are affordable.”
“We’ve created entirely new models of paying for curative HCV antivirals, and perhaps we need to be thinking the same thing for diagnostics,” says Greninger in a release.
The study appears in the Journal of Clinical Microbiology and received no external funding, supported instead by the Department of Laboratory Medicine and Pathology at the UW School of Medicine.
Photo caption: Illustration of finger-stick blood draw for hepatitis C testing with inserted sketch of the virus.
Photo credit: Alice C. Gray