Smartphone-based system aims to enable patient self-application and remote monitoring of contact dermatitis tests, potentially expanding access to specialized care.
Mayo Clinic researchers are developing an artificial intelligence-powered tool designed to automate skin allergy patch testing, allowing patients to self-administer tests and use smartphone cameras to monitor reactions over time.
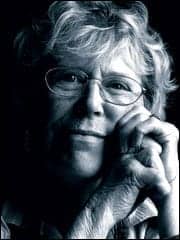
The technology, led by Alison Bruce, MB, ChB, a dermatologist at Mayo Clinic’s Jacksonville facility, aims to address current limitations in contact dermatitis diagnosis, which typically requires multiple office visits and specialized dermatology expertise that may be limited in rural areas.
“We’ve been working on an AI tool to help with skin allergy testing because, in current state, if you suspect that, as a patient or your doctor suspects that, you have allergic contact dermatitis, the way to test for that would be through patch testing,” says Bruce in a release.
Addressing Diagnostic Workflow Challenges
Traditional patch testing for contact dermatitis requires patients to visit dermatology offices multiple times. Patches containing potential allergens are applied to the skin, and then patients must return for readings at specific intervals to determine which substances trigger reactions.
The AI-powered system would enable patients to apply test patches themselves, remove them at predetermined times, and capture images using smartphone cameras. The artificial intelligence component would then analyze the images to identify positive reactions.
“Enhancing testing with AI would allow you to put the patches on your skin yourself, remove them at a predetermined time, and then use the camera on your phone to capture images,” Bruce says in a release. The AI could then interpret reactions, such as identifying a red reaction corresponding to nickel allergy.
Potential Market Impact
Contact dermatitis affects millions of patients annually and can be triggered by common substances including jewelry metals, fragrances, cosmetics, and topical medications. Current diagnostic workflows often create bottlenecks in dermatology practices due to the need for multiple patient visits and specialized interpretation expertise.
The smartphone-based approach could potentially expand testing capacity by reducing the burden on specialized dermatology staff while maintaining diagnostic accuracy. This could be particularly valuable for laboratories and healthcare systems serving rural populations with limited access to dermatology specialists.
Bruce notes that the technology could improve patient access by “making diagnosis more accessible and faster for patients,” particularly those in underserved geographic areas.
Image courtesy of Mayo Clinic