Summary:
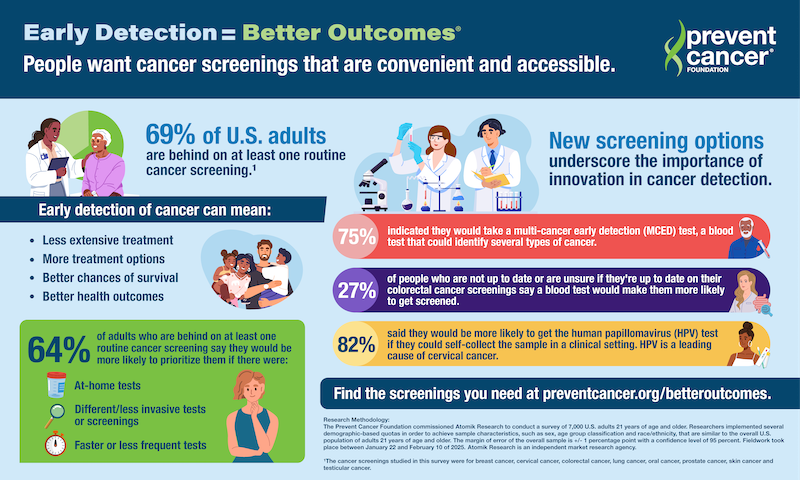
A new survey by the Prevent Cancer Foundation reveals declining cancer screening rates among U.S. adults, but shows strong interest in innovative, more convenient screening methods like at-home and multi-cancer early detection (MCED) tests.
Takeaways:
- Innovation is key: 64% of adults behind on screenings would be more likely to participate if given less invasive, faster, or at-home options.
- MCED potential: While awareness of multi-cancer early detection blood tests remains low, 75% of respondents said they would take one after learning more.
- Access matters: Convenience, such as self-collection options and home-based tests, could significantly improve screening uptake, especially for cervical and colorectal cancers.
U.S. adults report that their routine cancer screening rates are on the decline—but there is hope on the horizon. New screening technologies could encourage them to prioritize their screenings. According to the Prevent Cancer Foundation’s 2025 Early Detection Survey, 64% of adults who are behind on at least one routine cancer screening say they would be more likely to prioritize screening if there were innovative options such as an at-home test, a different/less invasive test or screening, a faster test or a less frequent test.1
These data highlight an urgent need for new screening options and underscore the importance of innovation in cancer detection.
Multi-Cancer Early Detection Could Unlock Better Health Outcomes
Multi-cancer early detection (MCED) testing—blood tests which have the potential to identify the presence of cancer for more than one cancer at a time—could be the key to unlocking better health outcomes for all. But awareness of MCED tests remains relatively stagnant from last year, with 42% saying they have heard of MCED tests but don’t know much about them. After reading more information about MCED tests, however, 75% of participants indicated they would take an MCED test. While MCED tests are designed to be complementary to—not a replacement for—existing routine cancer screenings. FDA approval of these tests, along with insurance coverage, could lead to increased screening rates. To support Medicare’s ability to evaluate coverage for new innovations following FDA approval, the Foundation continues to advocate for the passage of the Medicare Multi-Cancer Early Detection Screening Coverage Act.
Other approaches to screening, such as tests that can be done from the comfort of one’s home, are another potential way to increase screening rates. Earlier this year, the U.S. Food and Drug Administration (FDA) approved a first-of-its-kind, at-home human papillomavirus (HPV) test to screen for the virus that causes the majority of cervical cancers.
This comes just one year after the FDA’s approval of HPV self-collection in a health care setting. Survey participants cited not having the time (busy schedule) and lack of reliable transportation as reasons they were not getting screened. But when given information about the option to self-collect at a clinic, 82% of respondents eligible for cervical cancer screening said they would be more likely to get their cervical cancer/HPV screening.
Additional Approaches Needed for Cancer Screenings
The need for innovation extends far beyond cervical cancer—additional approaches to screening are essential for all cancer types. Among those who are either not up to date or who are unsure if they are up to date on their colorectal cancer screening, more than a quarter (27%) say they would be more likely to prioritize their screening if there were an option to screen for colorectal cancer with a blood test.
“Behind every data point is a person—and what they’re telling us is clear: They want cancer screenings that are convenient and accessible,” says Jody Hoyos, CEO of the Prevent Cancer Foundation. “It’s time we truly listen; we need to raise awareness about all available options and meet people where they are—supporting their lifestyles and helping to reverse the trends we’re seeing. And we need to fund research to discover the best screening methods for all cancer types, as well as ensure people have information and access to the effective screening methods available now. New breakthroughs in cancer screenings can lead to a world where cancer is preventable, detectable and beatable for all.”
Exciting advancements in early detection are already reshaping the future of screening. From AI-powered tools to groundbreaking non-invasive tests, researchers are pushing the boundaries of innovation to make screenings both effective and available in more settings. These breakthroughs could revolutionize how we detect cancer, ensuring more people get screened earlier and more conveniently than ever before.
Early Detection = Better Outcomes
The Prevent Cancer Foundation is dedicated to equipping people with the tools they need to check their health and stay ahead of cancer. If you don’t know where to start, check out the Foundation’s list of screenings you need at every age, free and low-cost cancer screening resources and a tool to create your own personalized screening plan.
Information and resources on all cancer types studied in the 2025 Early Detection Survey—including information on relevant screenings—can be found at preventcancer.org/betteroutcomes.
Research Methodology
The Prevent Cancer Foundation commissioned Atomik Research to conduct a survey of 7,000 U.S. adults 21 years of age and older.1 Researchers implemented several demographic-based quotes in order to achieve ample characteristics, such as sex, age group classification, and race/ethnicity, that are similar to the overall U.S. population of adults 21 and older. The margin of error of the overall sample is +/- 1 percentage point with a confidence level of 95%. Fieldwork took place between January 22 and February 10 of 2025. Atomik Research is an independent market research agency.
Featured Image: Early detection of cancer leads to better outcomes for patients. Image: Prevent Cancer Foundation
1The cancer screenings studied in this survey were for breast cancer, cervical cancer, colorectal cancer, lung cancer, oral cancer, prostate cancer, skin cancer and testicular cancer.