A board of pathology experts appeals for collaboration to improve patient care
Interview by Steve Halasey
At the end of February, a group of anatomic pathology experts from leading healthcare institutions around the globe gathered at the Tucson headquarters of Ventana Medical Systems Inc to examine laboratory-based patient safety issues and work toward a consensus on how to advance the standard of care for patients.
In the press release announcing the formation of the advisory board, Ventana hinted at the scale of current patient safety concerns in anatomic pathology labs. In the United States, 8% of tissue slides are cross-contaminated during the traditional hematoxylin and eosin (H&E) staining process, and more than 1 in 100 slides are misidentified due to human error.
Convened by Ventana as the International Pathology Patient Safety Advisory Board, the group that gathered in February was charged to review current patient safety issues with a focus on such matters as:
- The current state of patient safety in anatomic pathology, including key unmet needs.
- Perspectives on how additional industry guidelines could improve patient care.
- Technology’s role in improving quality and the patient safety standard of care.
[reference id=”37043″]Principles for Pathology and Patient Safety[/reference]
The first meeting of the board ended with adoption of four principles for guiding patient safety improvements in pathology laboratories worldwide (see sidebar). To find out more about the board and its recommendations, CLP spoke with Dr. Eslie Dennis, MBChB, vice president of scientific affairs for Ventana and chair of the advisory board.
CLP: How well is the quality performance of anatomic pathology labs currently being documented?
Dr. Eslie Dennis, MBChB: Organizations such as the College of American Pathologists (CAP) and the International Organization for Standardization (ISO) have developed numerous standards and guidelines to define quality practices that contribute to patient safety. These groups and their committees have been charged to develop integrated approaches to improving patient safety with respect to lab medicine and patient safety goals. However, their recommendations have been quite broad.
Let me give you an example. The ISO 15189 requirements for quality and competence in medical laboratories state that procedures shall be in place to prevent cross-contamination. CAP has equivalent checklists. But the recommendations are quite broad, and we need more-specific recommendations about how to standardize these procedures and the related documentation.
So, although quality testing is strictly enforced by accreditation agencies, standardization of a quality path has to be put in place to ensure that all labs—from office to large reference labs—perform quality testing in the same way.
The consensus of our advisory board was that failures in lab quality related to patient safety are likely under-recognized and under-reported, and that even when unfavorable outcomes occur, they are not necessarily made known publicly.
In response to this, the board identified a need for the pathology community to develop and implement common policies and procedures for documenting, investigating, and reporting safety incidents.
CLP: Outside of regulatory pathways, is laboratory quality performance the subject of ongoing research and analysis?
Dennis: There are published research papers, and there continues to be ongoing research in this field, but there are challenges in ensuring transparency in data collection. One of the seminal studies in this area was the CAP Q-probes study published back in 1996 by Gordon N. Gephardt, MD, and Richard J. Zarbo, DMD, MD. That study provided a tremendous amount of data, benchmarking the prevalence and handling of extraneous tissue contaminants in 275 surgical pathology laboratories, mostly in the United States.
But today, we’re not certain that we would be able to gather this level of detailed information. The consensus of our advisory board was that this type of information would be hard to gather, as people are reluctant to report their errors—particularly when legal exposure is significant.
The advisory board recommended that further investigation, research, and data gathering need to be performed in order to lead to the development of guidelines and recommendations to improve and prevent such events. This is a topic we intend to explore further with our advisory board.
CLP: Beyond the error rates that you cited for slide contamination and misidentification, are there additional areas where lab quality performance has become an issue of concern?
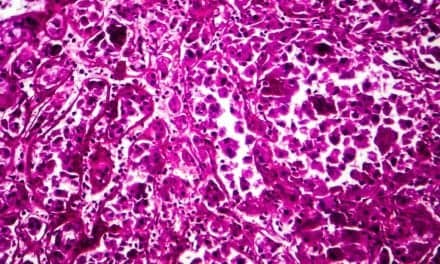
Dennis: Yes. The third area of great concern to the advisory board is that of tissue preservation. Anatomic pathology deals with patients’ tissue samples, which must be kept intact throughout the sample preparation and testing process that includes individual visual inspection and description, followed by processing, sectioning, and staining. This specialty area is therefore particularly vulnerable to errors from specimen mishandling, misidentification, and contamination.
Although most people today assume that the lab process is fully automated and “untouched by human hands,” this is not the case with anatomic pathology. There was strong agreement by the board members that avoiding these types of problems is a continuing challenge. The critical importance of specimen identification, integrity, and preservation create the need for increased adoption and use of automation and tracking systems.
Preanalytics start from the time a patient undergoes a procedure and specimens are obtained by surgeons in the operating room or through interventional procedures by other clinicians such as pulmonologists, gastroenterologists, and radiologists. Challenges arise from the number of manual touch points in the sequence. Each touch point increases the risk of contamination and misidentification.
Pathologists currently have no control over specimen-related activities outside the lab, and this makes standardization throughout the specimen chain of custody challenging. There are differences in local practices regarding specimen handling, labeling, and transport. And this highlights the need for hospital laboratory administrators to be involved with the many practices involving specimen submission to the lab.
We need to work together as a healthcare team to ensure standardization of routinely used procedures and checklists. As personalized medicine continues to grow, with the increasing role of companion diagnostics as the gateway to targeted therapies, it is vital that preanalytics and tissue fixation be standardized to preserve critical tissue components and deliver accurate, error-free patient diagnoses.
CLP: As a solution to these issues, how did the idea of convening an advisory board for improving anatomic pathology processes and to protect patient safety come about?
Dennis: Ventana was founded 27 years ago by a pathologist, Tom Grogan, who pioneered the automation and standardization of tissue biopsy testing specifically to address concerns in the anatomic pathology lab—including patient safety. Our mission at Ventana is to improve the lives of all patients afflicted with cancer. To do this, it’s imperative that the right diagnosis be made for the right patient every time.
We continue to build upon our mission by better understanding the current patient safety landscape—and by obtaining insights from advisory board members about future trends in patient safety—so that we can determine how best we, as a leader in the tissue diagnostics industry, can be proactive and contribute to improving quality in patient safety as a standard of care.
CLP: How were the members of the advisory board selected?
Dennis: There are many outstanding patient safety experts and champions. The advisory board members were selected due to their recognized expertise in the global pathology community and their availability. The board members come from the United States, Europe, Asia, and Australia. We wanted to get a global perspective on patient safety—not just the perspective from the US alone.
CLP: The principles developed by the board were presented during the annual meeting of the United States and Canadian Academy of Pathology (USCAP) at the beginning of March. What was the context of that presentation, and how did the audience respond?
Dennis: Our advisory board convened and developed the consensus statement a few days prior to the USCAP meeting. The group felt strongly that we should issue the consensus statement at USCAP. Because of the time frame we did not make a formal presentation, but we were able to release the statement and provide it to attendees of the meeting as a takeaway from the Ventana booth.
It’s been wonderful to see the positive response that this critical topic is generating. I’ve been approached to provide more details and in particular more information about next steps and how others can get involved.
CLP: As you’ve suggested, the preanalytic phase of anatomic pathology is a notoriously variable process. How does the advisory board propose to achieve standardized quality control in this very difficult area? Can procedural compliance followed by documented monitoring be implemented, as seems to be necessary?
Dennis: We fully agree that this is a highly variable process. With the advisory board, it is our intent to explore ways to reach a point where we do have standardized procedures and standardized documentation. We’re lacking those right now, and that’s an area that we have to be able to improve on.
We need to increase awareness of the issues and increase our ability to have dialogue across a number of different functions and stakeholders. Then, together with the board, we can explore ways to generate data that will help to drive changes in practice, and lead us to the point where we have standardized and documented procedures as well as guidelines that include standardized methods for both preventing errors and documenting them when they occur.
CLP: Will you or members of the board be presenting the principles at meetings of other pathology-related organizations?
Dennis: Yes. We will certainly be presenting these principles and discussing ways to continue to drive the momentum in this field with other pathology-related associations as well as other professional organizations and stakeholders, including patient organizations.
CLP: You’ve previously suggested that patient care will be markedly improved if these principles are widely embraced by stakeholders and the pathology community. But you’ve also indicated there are some challenges—including potential legal liabilities. How do you and the board expect that forward motion toward that goal might develop?
Dennis: We would like to increase awareness and forward the dialogue through engagement with other stakeholders, including surgeons, OR staff, clinicians, administrators, professional organizations, and patient safety organizations. For instance, we’re a proud sponsor of the National Patient Safety Foundation.
It’s our intention to continue meeting with the advisory board to explore ways to increase awareness, generate additional safety-related data to drive change, and identify additional opportunities to improve patient safety.
We would like to drive toward specific consensus recommendations and guidelines for improvements in preventative areas, and especially in how specifically to deal with and document errors in a standardized way. These guidelines are not available today, and we’d like to work toward supporting the generation and implementation of such standardized practices.
CLP: How can others become involved in the board’s efforts?
Dennis: To learn more about our patient safety activities, I encourage individuals to sign up for our newsletters and seek additional information at www.saferpath.org.
We would also like members of the pathology community to start dialogues within their own organizations. We hope they will examine their patient safety practices—and in particular their policies for identifying, tracking, documenting, and investigating patient errors; and their procedures for identifying problems early and ultimately for preventing errors.
We look forward to expanding our network, and we’re especially interested to learn of those who will be willing to collaborate with us as we develop ways to collect additional data and drive recommendations for change. People can reach us through the “Contact Us” tab on www.saferpath.org.
CLP: What is the next immediate step for you and the board?
Dennis: The next immediate step is for us to reconvene with our board, and those plans are in the works. I think this is a critical topic for us. We’re very excited about the enthusiasm from our board and the enthusiastic response that we’ve had. We look forward to continuing to share our news.
Steve Halasey is the chief editor of CLP.