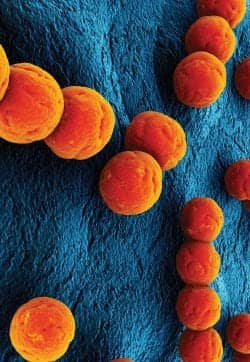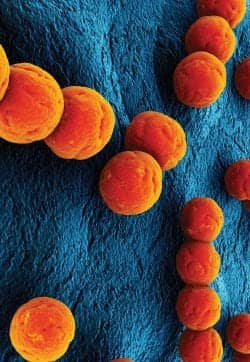
Hospital acquired infections (HAIs) affect at least one in 20 patients admitted for hospital care—which accounts for more than 1.5 million patients annually. The most common HAI is methicillin-resistant Staphylococcus aureus (MRSA), which affects more than 100,000 patients, causing more than 18,000 deaths each year. To put it into perspective, this number exceeds the death rate for breast cancer and AIDS combined.
Other “superbugs” are now creeping into hospitals, and there is an increased and ominous effect of these infections, including C. difficile, GBS, VRE, and other multiple drug-resistant organisms (MDROs). The organisms now can be found not just in hospitals and hospital-associated or health care-associated areas, but also in schools, playgrounds, gyms, and at beaches. The key question remains: How did HAIs come about?
BEFORE PENICILLIN
In the 1800s, infection and the spread of infection was considered to be via “poor ventilation” or “corruption of air.” General theory viewed personal hygiene as an unimportant means of preventing infection, as germ theory was still a questionable one.
Joseph Lister’s theory, which consisted of hand washing with carbolic acid to reduce infection prior to performing surgeries (limb amputations in particular), was popular in the 1880s and yielded an infection-reduction rate from 47% to 15%. Then there was Florence Nightingale’s demonstration that with scrub-brushed floors, fresh linens, and hand washing, infections in military hospitals during the 1854 Crimean War were reduced in half an hour from 40% to 2%—the current standard rate acceptable in modern surgical standards.
AFTER PENICILLIN
With the introduction of varieties of sulfas and other antibiotics, infection rates (surgical) were reduced to 2% by 1960. While Alexander Fleming discovered penicillin and its effect on bacteria, problems with isolation of penicillin hindered further exploration of the drug. However, by 1943, penicillin was readily available for World War II soldiers and was manufactured on a large scale.
Use of penicillin—proclaimed the “wonder drug”—expanded, but bacterial resistance to this drug rose significantly in just 3 years. In the 1940s, penicillin alternatives such as erythromycin and streptomycin, followed by methicillin (in the 1960s) and vancomycin, were introduced to combat bacterial infections. But, it takes just about a year and a half for organisms to develop resistance to these drugs (and their variations). Hospitals have improved their definitions of sterilization—including formaldehyde, alcohol, or ethylene oxide (gas), and have significantly decreased hospital infection rates.
SUPERBUGS
The advent of superbugs was apparent within decades. The overuse of antibiotics and overcautious prevention of infection in hospitals led to organisms developing resistance to available antibiotics. Some superbugs of concern today are vancomycin-resistant Enterococcus, Streptococcus, Klebsiella oxytoca, Serratia marescens, Pseudomonas aeruginosa, and Legionnaire’s disease. The death rate currently from superbugs is approaching ~90%, and they are responsible for more than 100,000 deaths each year.
DIAGNOSIS AND DETECTION
The Centers for Disease Control and Prevention (CDC) estimates that 1.7 million health care-acquired infections occur in US hospitals each year and are associated with 99,000 deaths. Disease detection, diagnosis, surveillance, prevention, and isolation appear to be the main factors that trigger streamlined products from cutting-edge molecular diagnostics and medical device companies.
HAI detection technology had been considered an almost orphan method. “Cepheid focused on health care-associated infection detection on purpose to address the demand in hospitals for these tests,” says David Persing, MD, PhD, executive vice president and chief medical and technology officer, Cepheid, Sunnyvale, Calif. “We intentionally avoided the standard disease-detection panels, such as CT/NG, HIV, HPV, HCV, etc, that every other diagnostics company was involved in.”
When Cepheid worked on the MRSA test, it was met with skepticism. However, “… if a diagnostics company using state-of-the-art molecular techniques does not have an HAI detection test on its panel now, it is deficient in its portfolio,” Persing adds.
Run on Cepheid’s GeneXpert system, Xpert MRSA/SA Skin and Soft Tissue Infection test (SSTI) is a rapid on-demand test for detecting MRSA and SA on skin and soft-tissue swabs in less than 1 hour. Most of Cepheid’s disease-detection portfolio is run on its GeneXpert system, which uses the company’s patented single-use cartridge system from sample preparation, extraction, and elution through amplification, with minimal hands-on time during the process.
With no human intervention during the process, a second confirmatory test can also be run as a confirmatory test, for precise diagnosis. The GeneXpert System is also used for other IVD products from Cepheid such as its Xpert C. difficile, Xpert EV, Xpert GBS, and Xpert MRSA/SA BC for testing MRSA and SA from positive patient blood culture bottles.
Similar to Cepheid in terms of walk-away automation and molecular diagnostics-based kits, BD Diagnostics, a segment of BD (Becton, Dickinson and Company), Franklin Lakes, NJ, has introduced in the United States its BD MAX ™ for use as an open system.


Most of Cepheid’s disease-detection portfolio is run on its GeneXpert system, which uses the company’s patented single-use cartridge system from sample preparation, extraction, elution through amplification, with minimal hands-on time during the process.
CDI
C. difficile infections in the United States range around half a million annually, with more than 25,000 deaths. The average hospital stay for a patient with C. difficile is three times longer than an average patient. A new strain, BI/NAP1/027, has been detected, and most diagnostics companies are focused on presenting sensitive tests for detection of this strain.
In January 2009, BD received its C. difficile detection molecular test clearance from the FDA (510(k) cleared CDI)—for the BD GeneOhm™ C. diff. molecular assay, the first C. difficile molecular test offering sensitivity and speed in a single test. The impetus behind this test was to improve patient care by reducing the need for multiple testing and avoiding unnecessary antibiotics.
In April 2011, Cepheid announced it received clearance from the FSA to market its Xpert® C. difficile /Epi test (its first C. difficile test has been in the US market since 2009), which is the tenth test in Cepheid’s Xpert panel to receive FDA clearance. “The test leading to detection of the 027 strain allows for identification in institutions that would be rapid, allowing for speed in isolation, diagnosis, surveillance, and treatment,” Persing says. John Bishop, Cepheid’s CEO, adds, “Since the 027 strain is associated with greater relapses and higher mortality rates, this test will be very beneficial for improved patient care.”
GBS
Group B Streptococcus (GBS) remains a leading cause of morbidity and infant mortality due to maternal colonization as a major risk for early-onset GBS. However, this health care-related infection is easily treatable with antibiotics during labor, provided the diagnosis is done early and precisely. Cepheid and BD Diagnostics provide easy and accurate diagnosis options for disease prevention.

BD Diagnostics recently introduced its BD MAX™ in the United States for use as an open system.

bioMérieux’s NucliSENS Easy Q MRSA test recently received clearance from the FDA.

The VITEK 2 card from bioMérieux contains 64 microwells and offers a comprehensive menu for the identification and antibiotic susceptibility testing of organisms.
In June 2010, BD Diagnostics announced the first 510(k) FDA–cleared test to detect GBS. By automating the process from sample lysis through PCR, the BD MAX system is a walk-away instrument, processing 24 samples in about 2 1/2 hours.
The direction of HAI detection should be perceived at a higher level, says one expert. “Not only does BD MAX allow for HAIs such as MRSA and C. difficile to be detected with accuracy in hours, it also allows for acceleration of therapy,” says Kathy Warye, vice president, infection prevention, at Becton Dickinson.
Not only do these tests detect the highly transmissible infections rapidly, but the test platform is open enough for the average lab or hospital setting to use for other tests, such as gastrointestinal infection panels or respiratory viral panels, she adds. According to BD, collaborations with other companies to yield tests on BD MAX will be beneficial for patients and hospital testing. BD, in collaboration with Diagenode, Denville, NJ, intends to develop seven assays focused on respiratory infections, viral- and parasite-based GI infections, and differential meningitis diagnosis.
MRSA
MRSA, one of the leading causes of HAIs in health care systems, is responsible for nearly 100,000 life-threatening infections and nearly 19,000 deaths each year, according to the CDC. MRSA is not just a hospital-and-health care-associated infection; it has also spread into the community.
France-based bioMérieux, with North American headquarters in Durham, NC, offers products for prevention, intervention, and surveillance of HAIs. Its range of chromogenic culture media is dedicated to MRDOs from clinical samples. “In the US, ChromID MRSA and ChromID VRE are among the popular media sold to microbiology labs,” says Narayan Krishnaswami, global product manager-nosocomial infections, at bioMérieux.
On May 23, the company’s NucliSENS Easy Q MRSA test received clearance from the FDA. The company also offers the PREVI Isola, an automated plate streaker for speeding microbiology testing. A combination of tests and reagents that screen and prevent disease transmission, these products help contain the infection and further isolate the organism.
Based on NASBA, bioMérieux’s MRSA test allows for simultaneous detection of the cassette junction and mec-A gene, detecting seven MRSA types. Up to 46 samples can be processed per run in just 3 hours. Batch processing efficiency increases dramatically with this footprint.
“Delivering relevant information faster for patient management and to enable prevention measures is an important goal for the company,” Krishnaswami says. “We’re focused on early detection, marker identification, and test development focused on how certain phenotypical expressions occur.”
Persing says that with the availability of very specific and sensitive tests such as Cepheid’s Xpert MRSA/SA SSTI and BC tests, the information is highly actionable. He expects more tests to be introduced in the market focused on VREs and multiresistant gram-negative MRDOs, where detection is key to survival (ie, patients with these infections are at their last lines of therapy).
“Rapid identification and diagnosis is required,” Persing says. “Cepheid’s tests are different in that the total time from sample to answer is 1 hour, and it doesn’t need to be batched.”
PARADIGM SHIFT: WHO WILL USE THESE TESTS?
This somewhat radical shift in testing may be difficult for large-hospital testing labs to implement. Persing notes that most of these tests can and should be used in small hospitals, and for urgent care with no batch testing (moderate-complexity CLIA centers). This may drive up test costs, with increased training for these tests. Would hospital directors be interested in such testing?
In collaboration with LABSCO, Louisville, Ky, a privately held supplier of clinical lab products to hospitals, physician’s office labs, and reference labs in the United States, Cepheid’s GeneXpert systems and tests will be placed in the acute care hospital market for hospital settings with less than 150 beds. “Labs have to see that while these tests cost money, overall they save money and improve bed management in hospitals,” Persing says. “CEOs and CFOs of hospitals will then be considered heroes if they impact health care positively by looking at the overall picture.
“For example, flu testing: If you test a patient in an hour, you don’t have to isolate them and spend bed space dollars. This guilty-until-proven-innocent theory ends up being very costly and needs to change,” Persing adds.
BD’s Warye agrees. “Our BD MAX platform has been greeted with great expectations in hospitals,” she says. “The idea is not only to run the tests we offer, but because of its open platform, large labs should be able to run their own tests.” These tests and instruments can be run by a lab technician rather than a trained medical technologist, and increase the ability of testing by mixing and matching assays with a run for cost-effective molecular testing.”
“Real-time PCR has yet to be a real-time diagnostic,” Persing says. “That is what we are offering to hospitals.”
GIVING BACK—AWARENESS OF HAIS
bioMérieux hosted the third World HAI Forum in June, convening experts from around the world for scientific discussions focusing on controlling antimicrobial resistance. In 2010, BD Diagnostics launched the BD Protect ™ Infection Surveillance and Prevention software portfolio, with health care management software solutions tracking infections and preventing their transmission. bioMérieux also has a surveillance software portfolio, but has not yet released it in the United States.
FUTURE OF HAIS
While testing improves, the MRDOs appear to shape shift with rapidity. The next stage of HAI detection and prevention would be not only in molecular diagnostics testing, but also in radically changing hospital and health care settings. Since these infections are now also community-acquired, as a society we have to evaluate the standards of what is considered germ-free and how it affects health care.
Prevention may be the best cure. However, we have become an overprevention society, which had led to a new disease breed. It may be time to rethink our strategy of prevention, cure, and surveillance.
Madhushree Ghosh, PhD, is a San Diego-based science and health writer.