Summary: Lynx Dx announces the at-home availability of MyProstateScore 2.0 (MPS2), a highly accurate urine-based prostate cancer test that eliminates the need for a digital rectal exam (DRE), expanding access and reducing unnecessary biopsies.
Key Takeaways:
- Greater Accessibility: The at-home version of MPS2 allows men to collect urine samples conveniently, improving access to prostate cancer screening, especially for those in remote or underserved areas.
- High Diagnostic Accuracy: Published in The Journal of Urology, MPS2 demonstrates 91–94% sensitivity for detecting clinically significant prostate cancer and reduces unnecessary biopsies by identifying up to 53% of men with negative results.
- Seamless Telehealth Integration: With stable urine samples that don’t require temperature control, MPS2 supports modern telehealth practices, enabling more patient-centered and flexible prostate cancer risk assessment.
Lynx Dx, a leader in innovative diagnostic solutions, announced today that its pioneering MyProstateScore 2.0 (MPS2) will be made available for at-home sample collection, enabling broader accessibility and helping more men safely avoid biopsies.
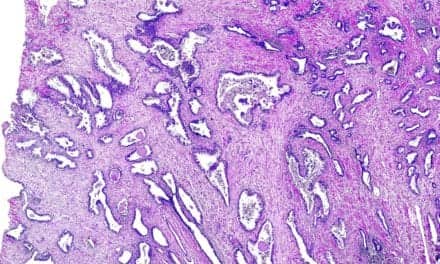
The news follows the study published in the Journal of Urology, which found that MPS2 delivers high accuracy in predicting clinically significant prostate cancer using urine collected without a preceding digital rectal exam (DRE). This advancement further establishes MPS2 as a transformative tool in prostate cancer screening, offering unparalleled diagnostic flexibility and patient convenience without compromising accuracy.
The at-home version of MPS2 is expected to be available for ordering in February.
Unmet Need
Prostate cancer remains a significant health challenge, being the second leading cause of cancer-related deaths in American men. Traditional screening methods often lead to excessive biopsies, overdiagnosis of low-grade cancer, and patient discomfort. Lynx Dx aims to address these challenges with the MPS2 test, which is designed to accurately assess the risk of clinically significant prostate cancer while reducing exposure to risks associated with biopsies.
“Lynx Dx is proud to offer a solution that provides men with a more convenient, accessible, and accurate option for prostate cancer screening,” says Spencer Heaton, MD, chief medical officer at Lynx Dx. “By eliminating the need for a DRE, MPS2 now empowers patients to collect their samples in the comfort of their homes, a significant step forward in prostate cancer risk assessment and our commitment to patient-centered care.”
Further Reading
Validated Accuracy, Unprecedented Flexibility
Published data from The Journal of Urology demonstrate the accuracy of MPS2 in predicting the risk of clinically significant prostate cancer using urine collected without the need for a DRE, paving the way for convenient at-home and telehealth applications. The study demonstrated that MPS2 significantly outperformed traditional prostate-specific antigen (PSA) testing by identifying up to 53% of men whose biopsy would be negative while maintaining 91–94% sensitivity for high-grade cancer (Grade Group ≥2).
Patients now have the flexibility to complete the MPS2 test without a DRE in-office or at home, ensuring compatibility with modern telehealth practices and improving access for individuals in remote or underserved areas. The collected urine samples are stable without temperature control or special packaging, ensuring reliable results. Because of this stability, patients can ship their samples any day of the week without worrying about degradation.
“The ability to collect MPS2 samples at home without requiring a digital rectal exam empowers patients and providers with a test that is both convenient and precise,” says Ganesh S. Palapattu, MD, FACS, FRCS. “By enhancing patient comfort and optimizing clinical workflows, this approach aligns with the evolving needs of modern healthcare. Our findings show that this method maintains the high accuracy and efficiency of MPS2, which continues to set the standard for accurate, efficient prostate cancer risk assessment, exemplifying how innovation and accuracy can go hand in hand.”