With new guidelines for diagnosis, treatment, and prevention, healthcare providers are keeping C. diff in their sights.
By Sherry Dunbar
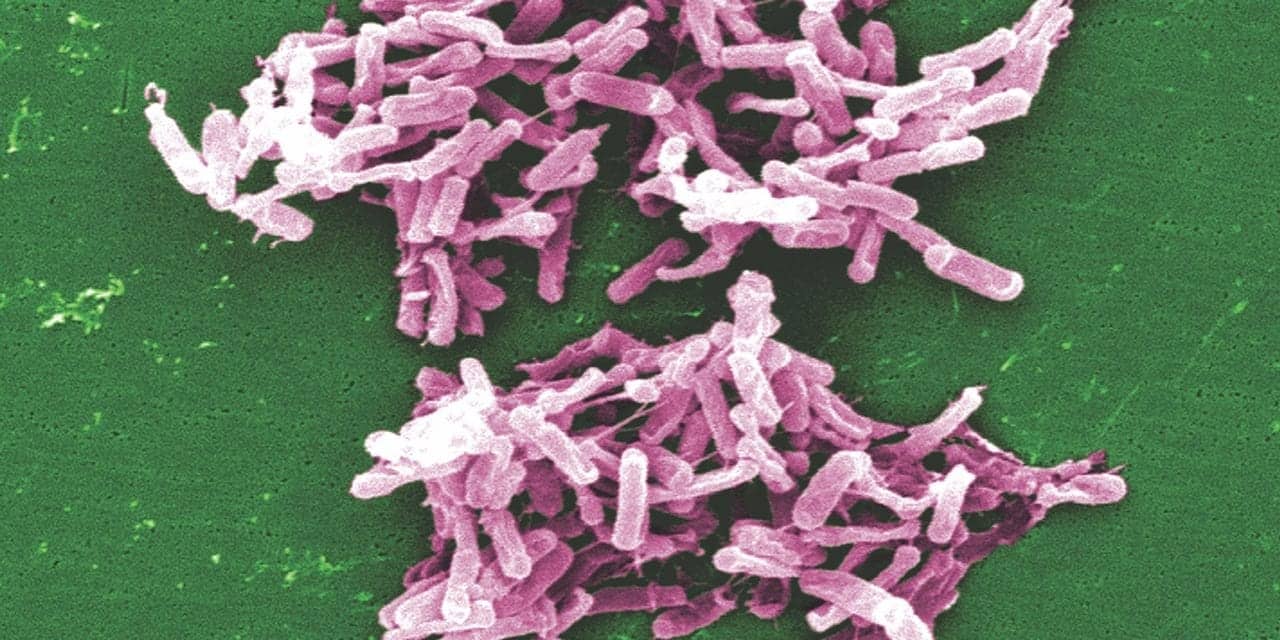
Among healthcare-associated infections, Clostridioides difficile (C. diff) represents a major threat to public health. In the United States alone, almost half a million C. diff infections are diagnosed each year, with nearly 30,000 of those infected patients dying within a month of diagnosis.1 This pathogen is now responsible for the greatest number of healthcare-associated infections seen in the country.2
This crisis has spurred increased activity toward improving the ways we test for and treat C. diff. Recently, the Infectious Diseases Society of America (IDSA) and the Society for Healthcare Epidemiology of America (SHEA) issued new clinical guidelines featuring a number of important changes in how medical professionals should address C. diff infections. This resource will make it possible for healthcare teams to respond more effectively and reduce the incidence of nosocomial C. diff cases.
On other fronts, clinical research teams are making progress with new studies that are shedding light on approaches to testing and patient care protocols. Some studies have looked more closely at policies associated with C. diff patients, such as isolation protocols for asymptomatic carriers and universal screening of all patients admitted to hospitals.3,4 Neither of these approaches is currently considered standard practice at most institutions, but this new research will be essential for developing better and more cost-effective means of containing the pathogen and preventing its transmission within healthcare facilities.
In another example, extensive research has demonstrated that molecular tests focused on NAP1, a marker specific to one strain of C. diff, are becoming less helpful now that other strains are increasingly common sources of infection.5–7 This data is critical as labs seek to calibrate their testing processes for the best results among their patient populations.
Collectively, these new guidelines and hospital research could help clinical labs and other healthcare professionals significantly improve testing and treatment for patients with C. diff infections.
IDSA/SHEA Guidelines
The recently released IDSA/SHEA clinical guidelines for diagnosing, treating, and preventing C. diff infections are a much-needed resource to replace the nearly decade-old guidelines healthcare professionals have been using until now.8 This new look at best practices for C. diff reflects growing concerns about reining in the spread of this dangerous pathogen.
The latest guidelines include several major changes to how patients with C. diff infections should be treated. For instance, the use of metronidazole—long considered the first-line treatment for C. diff cases—is no longer preferred due to results from new clinical trials. IDSA/SHEA guidelines now strongly recommend vancomycin or fidaxomicin, given in a 10-day course, for adults with mild or moderate infections. For children, metronidazole is still the recommended treatment. For the one in four C. diff patients who experience recurring infections, IDSA and SHEA encourage a 10-day course of fidaxomicin or a tapered course of vancomycin over several weeks. Patients whose C. diff infections have recurred at least twice may be suitable candidates for fecal transplants, according to the new guidelines. And while IDSA and SHEA contend that there is too little clinical evidence to determine the utility of probiotics for preventing reinfection among C. diff patients, the organizations note that healthcare professionals may consider probiotics as part of a multifaceted treatment approach.
In addition to treatments, the IDSA/SHEA guidelines offer key insights into testing patients suspected of having a C. diff infection. Clinical experts acknowledge a real diagnostic challenge in these cases—after all, detecting the presence of C. diff is not necessarily sufficient to prove that this pathogen is the cause of disease, rather than a harmless presence in the patient’s intestinal flora. As the guidelines point out, the use of molecular diagnostics, which are unable to distinguish between a causal pathogen and a benign bystander, could overestimate the number of cases of C. diff.
To avoid inaccurately attributing infections to this pathogen, the guidelines establish very clear rules for when to test and when not to test patients for C. diff. For example, patients should only be tested for this pathogen when their diarrhea began recently with no other explanation, and they have had three or more bouts of diarrhea within 24 hours. The new protocols also clarify that patients who have received a negative result on a C. diff test should not be tested again until at least a week has passed. For children, the IDSA/SHEA guidelines recommend no C. diff testing at all when patients are less than a year old; for patients between 1 and 2 years of age, testing is only recommended when other common causes of diarrhea have been explored and dismissed. For all patients tested, protocols restrict sample type to diarrhea and not formed stool.
Importantly, the IDSA/SHEA guidelines do not highlight specific types of C. diff tests to use; that choice is left to the laboratory. Broadly though, the protocols do offer advice about the implementation of molecular diagnostics. These tests, which can return results much more quickly than other types of tests, are recommended for use with patients believed to have a C. diff infection (Figure 1). For hospitals that use the same test for suspected cases and for more general patient screening, IDSA and SHEA prefer the implementation of molecular tests in combination with advanced toxin tests to help identify patients for whom C. diff is actually causing an infection.
Clinical Research
Testing algorithms for C. diff have become less straightforward with the growing recognition that more people are harmlessly colonized with this microbe than ever suspected (Table 1).9 Indeed, evidence now shows that almost 30% of people routinely carry C. diff, even though they appear completely asymptomatic.10 Accurate testing is essential, but there is just as much need to prevent the misdiagnosis of patients who carry C. diff, but whose illnesses are caused by something else.
Still, the realization that C. diff is so widespread in the community is useful information for healthcare professionals and laboratorians alike. Colonized patients may serve as a reservoir for this pathogen, where asymptomatic people could pass the microbe on to other people. For that reason, some institutions have been trying out methods that involve universal C. diff screening for all patients admitted to a healthcare facility, followed by isolation protocols for people with positive results.
This was the case in a Canadian study in which clinicians evaluated the frequency of healthcare-associated infections in a 354-bed acute care facility, comparing results with screening and isolation to previous data in the same facility (Table 2).3 In the study, they found that the incidence of nosocomial C. diff infections was cut by more than half, starting at 6.9 cases per 10,000 patient-days and dropping to 3.0 cases per 10,000 patient-days, with the new protocols. Interestingly, the same study also examined the effects of these changes on healthcare costs. By analyzing the data, the clinicians predicted that the screening-and-isolation method prevented 62% of nosocomial C. diff infections, potentially saving as much as $627,000 in patient care costs over a 17-month period.
These results were supported by a study in Denmark designed to quantify C. diff infection rates before and after the implementation of screening and isolation protocols (Table 3).4 Conducted in two university hospitals, the study found that patients who were not exposed to carriers of C. diff were less likely to develop their own C. diff infections. Prior to these protocols, 4.6% of patients exposed to asymptomatic carriers developed C. diff infections; with the protocols, just 2.6% of patients exposed to carriers did so.
Clearly, there is much to be gained by gathering information about C. diff colonization as early as possible—that is, by screening patients upon admission to a hospital—and by taking care to isolate carriers so that they do not contribute to the rising incidence of nosocomial C. diff infections.
NAP1 Marker Testing
Molecular diagnostics for C. diff are not all designed the same (Figure 2). Different tests target various selections of organism ribotypes. Like any circulating infectious disease, new strains evolve over time; each particular ribotype may come and go. In the early 2000s, an epidemic of one ribotype—BI/NAP1/027—took place in North America and Europe, causing a major shift in C. diff epidemiology. Naturally, some test developers chose to include or even focus on this ribotype. However, the prevalence of this ribotype has waned in recent years as other strains have gained ground, and not all tests have kept up.
Some emerging C. diff strains, such as ribotype 244, appear to be closely related to the BI/NAP1/027 ribotype. These newer strains are making it tougher to accurately identify strains. Ribotype 244, for instance, is often misidentified as BI/NAP1/027 by some molecular diagnostics.11 These trends are currently causing more false positives for NAP1 and decreased specificity for these tests.12
Meanwhile, epidemiological surveillance has found that other ribotypes are rapidly becoming more common than BI/NAP1/027. A study of more than 650 C. diff isolates collected during a clinical trial in six different regions of the United States from 2010 to 2014 showed that ribotype frequency changed significantly over time.5 Within the populations selected for study, researchers found that the BI/NAP1/027 ribotype was seen as often as 43% of the time in 2010 but dropped to a frequency of just 14% by 2014. Meanwhile, ribotypes such as 014/020, 106, and 002 became more prevalent.
The trend holds in other countries as well. A study in Canada found that NAP1 isolates dropped in frequency by 29% from 2008 to 2013.6 According to a European study spanning nearly 1,200 clinical isolates collected from nearly 500 hospitals and almost 20 countries, the ribotypes seen most often were BI/NAP1/027 (19%), 001/072 (11%), and 014/020 (10%).7 The data, reflective of patient cases in 2012 and 2013, diverged dramatically from a 2008 study; only the 014/020 ribotype was consistently seen as one of the three most frequent strains. The BI/NAP1/027 ribotype, which had been seen most often in the UK and Ireland in 2008, was 5 years later less prevalent in those countries but had become more common in Germany and Eastern Europe.
This shifting ribotype landscape suggests that focusing C. diff testing on detection of the NAP1 marker would be short-sighted. While identifying this ribotype may be somewhat helpful for disease prognosis, the strain is usually treated with the same protocols as most other infection-inducing C. diff strains. Instead of making testing specific to this ribotype, a better approach would be relying on patient history and symptoms along with IDSA/SHEA clinical guidelines to make sure that each patient receives the best care, regardless of whether the causal strain includes the NAP1 marker.
Moving Forward
Taken together, the IDSA/SHEA clinical guidelines, paired with results about hospital policy implementation and C. diff strain prevalence, offer a path forward in the ongoing effort to address this deadly healthcare-associated infection. New testing approaches and isolation protocols could help reduce the transmission of C. diff in hospitals and other healthcare settings. By improving testing algorithms and selecting assays that deliver the needed information either for screening or for suspected cases, clinical laboratorians have an important role to play in optimizing patient outcomes.
Sherry Dunbar, PhD, MBA, is senior director of global scientific affairs at Luminex. For further information, contact CLP chief editor Steve Halasey via [email protected].
References
- Clostridioides difficile Infection [online]. Atlanta: Centers for Disease Control and Prevention, 2019. Available at: www.cdc.gov/hai/organisms/cdiff/cdiff_infect.html. Accessed January 31, 2019.
- Magill SS, Edwards JR, Bamberg W, et al. Multistate point-prevalence survey of healthcare-associated infections. N Engl J Med. 2014;370:1198–1208; doi: 10.1056/nejmoa1306801.
- Longtin Y, Paquet-Bolduc B, Gilca R, et al. Effect of detecting and isolating Clostridium difficile carriers at hospital admission on the incidence of C difficile infections: a quasi-experimental controlled study. JAMA Intern Med. 2016;176(6):796–804; doi: 10.1001/jamainternmed.2016.0177.
- Blixt T, Gradel KO, Homann C, et al. Asymptomatic carriers contribute to nosocomial Clostridium difficile infection: a cohort study of 4508 patients. Gastroenterology. 2017;152(5):1031–1041.e2; doi: 10.1053/j.gastro.2016.12.035.
- Snydman DR, McDermott LA, Jenkins SG, et al. Epidemiologic trends in Clostridium difficile isolate ribotypes in United States from 2010 to 2014. Open Forum Infect Dis. 2017;4(Suppl 1):S391; doi: 10.1093/ofid/ofx163.973.
- Jassem AN, Prystajecky N, Marra F, et al. Characterization of Clostridium difficile strains in British Columbia, Canada: a shift from NAP1 majority (2008) to novel strain types (2013) in one region. Can J Infect Dis Med Microbiol. 2016;2016:8207418; doi: 10.1155/2016/8207418.
- Davies KA, Ashwin H, Longshaw CM, Burns DA, Davis GL, Wilcox MH. Diversity of Clostridium difficile PCR ribotypes in Europe: results from the European, multicenter, prospective, biannual, point-prevalence study of Clostridium difficile infection in hospitalized patients with diarrhea (EUCLID), 2012 and 2013. Euro Surveill. 2016;21(29); doi: 10.2807/1560-7917.es.2016.21.29.30294.
- McDonald LC, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018;66(7):e1–e48; doi: 10.1093/cid/cix1085.
- Hung YP, Lee JC, Lin HJ, et al. Clinical impact of Clostridium difficile colonization. J Microbiol Immunol Infect. 2015;48(3):241–248; doi: 10.1016/j.mii.2014.04.011.
- Lessa FC, Mu Y, Bamberg WM, et al. Burden of Clostridium difficile infection in the United States. N Engl J Med. 2015;372:825–834; doi: 10.1056/nejmoa1408913.
- Lim SK, Stuart RL, Mackin KE, et al. Emergence of a ribotype 244 strain of Clostridium difficile associated with severe disease and related to the epidemic ribotype 027 strain. Clin Infect Dis. 2014;58(12):1723–1730; doi: 10.1093/cid/ciu203.
- Kociolek LK, Gerding DN. Clinical utility of laboratory detection of Clostridium difficile strain BI/NAP1/027. J Clin Microbiol. 2016;54(1):19–24; doi: 10.1128/jcm.02340-15.