A new study found rapid antigen detection tests for SARS-CoV-2 proved more effective than expected when compared with virus detection rates using the established standard test, the polymerase chain reaction (PCR) assay.
Researchers at Johns Hopkins Medicine, the University of Maryland Medical Center, the University of Maryland School of Medicine and four other collaborators conducted the study which involved some 6,000 patients seen at the Baltimore Convention Center Field Hospital (BCCFH) during a 10-day period around the beginning of 2021
The study was first posted online in the American Society for Microbiology journal Microbiology Spectrum.
“We found that virus was accurately detected by the rapid antigen test in 87% of patients with COVID-19 symptoms and in 71% of those who were asymptomatic — rates that surprised us because they were so high,” says study lead author Zishan Siddiqui, MD, assistant professor of medicine at the Johns Hopkins University School of Medicine. “This is a significant finding because the rapid test offers a number of advantages over the PCR test, including time savings, both in sampling and processing; cost savings; and most importantly, ease of distribution and application — basically anywhere — which can help overcome COVID testing disparities in medically underserved communities.”
The first step for both the PCR and rapid antigen tests is obtaining a sample from a patient, either a nasal swab or a bit of saliva. The difference lies in how the sample is processed and analyzed. A PCR test takes a tiny bit of SARS-CoV-2 genetic material from a sample and reproduces it thousands of times so it can be more easily detected. A rapid antigen test uses laboratory-produced antibodies to seek out and latch onto proteins on the surface of SARS-CoV-2 particles in the sample.
The PCR test requires a skilled laboratory technician, special equipment and up to an hour or more to process. Additionally, testing on a massive scale can only be conducted at a large, centralized testing facility, such as a hospital laboratory.
On the other hand, rapid antigen testing uses a premade kit with a reagent that contains antibodies specific for SARS-CoV-2. The test can be conducted by anyone after brief training, can be administered anywhere, and provides results in approximately 15 minutes.
“What we determined was that while the PCR test may be a better test from a clinical perspective—as it’s basically 100% accurate at detecting SARS-CoV-2—the rapid antigen test appears to be better from a public health standpoint because of its ease of use, and the fact that it proved to have sufficient accuracy, specificity and reliability for detecting the coronavirus in a high-volume setting,” says study senior author James Ficke, MD, professor of orthopaedic surgery at the Johns Hopkins University School of Medicine and co-director of the BCCFH for 16 months. “The field hospital was the perfect place to determine this because we could see how well both tests worked for a large number of people in a short amount of time.”
In a future study, the researchers plan to assess the accuracy of rapid antigen tests being marketed for home use.
“Our successful program has shown that a health care system can provide an equitable response to COVID-19 because the rapid antigen test makes it possible to test all socioeconomic levels of a large population quickly and repeatedly — and this has become the model that the state of Maryland is actively putting into practice and other organizations are starting to follow,” says Ficke.
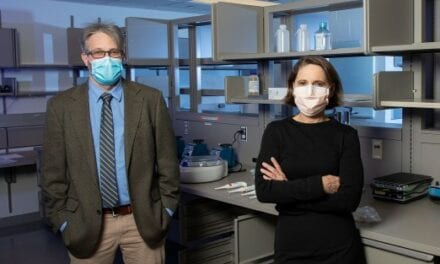
Featured Image: Researchers at Johns Hopkins Medicine and collaborators report that a rapid antigen detection test for SARS-CoV-2, the virus that causes COVID-19, proved more effective than expected when compared with virus detection rates using the established standard test, the polymerase chain reaction (PCR) assay. Photo: Graphic created by M.E. Newman, Johns Hopkins Medicine, using public domain images.