Summary: Researchers have developed a low-cost, paper strip test using CRISPR technology that can quickly and accurately diagnose various influenza strains, potentially improving outbreak response and clinical care.
Takeaways:
- The paper strip test is low-cost and can be used outside of traditional laboratory settings, making flu diagnosis more accessible.
- The test uses SHINE technology with CRISPR enzymes to distinguish between influenza A, B, and various subtypes, and can identify strains resistant to antiviral treatments.
- The test provides results in about 90 minutes at room temperature, with potential future improvements to deliver results in 15 minutes, enhancing both clinical care and epidemiological surveillance.
Fewer than one percent of people who get the flu every year get tested, in part because most tests require trained personnel and expensive equipment. Now researchers have developed a low-cost paper strip test that could allow more patients to find out which type of flu they have and get the right treatment.
Paper Strip Test for Influenza
The test, developed by a team from the Broad Institute of MIT and Harvard and Princeton University, and supported by the US Centers for Disease Control and Prevention, uses CRISPR to distinguish between the two main types of seasonal flu, influenza A and B, as well as seasonal flu subtypes H1N1 and H3N2. It can also identify strains that resist antiviral treatment, and with further work, could potentially detect swine and avian flu strains, including H5N1, which is currently infecting cattle.
Appearing in The Journal of Molecular Diagnostics, the results could help improve outbreak response and clinical care by bringing tests that are accurate, low-cost, and fast to doctors’ offices and labs across the US and in other countries.
“Ultimately, we hope these tests will be as simple as rapid antigen tests, and they’ll still have the specificity and performance of a nucleic acid test that would normally be done in a laboratory setting,” says Cameron Myhrvold, co-senior author on the study along with Pardis Sabeti, an institute member at the Broad and a professor at Harvard University and the Harvard T.H. Chan School of Public Health, as well as a Howard Hughes Medical Institute investigator. Myhrvold, who is currently an assistant professor at Princeton University, was a postdoctoral researcher in Sabeti’s lab when the study began.
Test Uses CRISPR Enzymes
The test is based on a technology called SHINE, which was developed by Sabeti’s lab in 2020 and uses CRISPR enzymes to identify specific sequences of viral RNA in samples. The researchers first used SHINE to test for SARS-CoV-2, and later to distinguish between the Delta and Omicron variants. Then, in 2022, they began adapting the assay to detect other viruses they knew were always circulating: influenzas. They wanted to create tests that could be used in the field or in clinics rather than hospitals or diagnostic labs with expensive equipment.
“Using a paper strip readout instead of expensive fluorescence machinery is a big advancement, not only in terms of clinical care but also for epidemiological surveillance purposes,” says Ben Zhang, co-first author on the study, a medical student at Harvard Medical School and an undergraduate researcher in Sabeti’s lab when the study began.
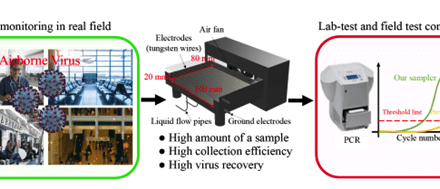
Typical diagnostic approaches such as polymerase chain reaction (PCR) require lengthy processing times, trained personnel, specialized equipment, and freezers to store reagents at -80°C, whereas SHINE can be conducted at room temperature in about 90 minutes. Currently, the assay only requires an inexpensive heat block to warm the reaction, and the researchers are working to streamline the process with the goal of returning results in 15 minutes.
The researchers also adapted SHINE to distinguish between different flu strains. In the future, they say the assay could be adapted to detect two different viruses with similar symptoms, such as influenza and SARS-CoV-2.
“Being able to tease apart what strain or subtype of influenza is infecting a patient has repercussions both for treating them and public health interventions,” says Jon Arizti-Sanz, a postdoctoral researcher in Sabeti’s lab and co-first author on the study.
For example, the tests could help clinicians decide whether to use Oseltamivir, a common antiviral that is effective for only some strains, Arizti-Sanz added. In the field, rapid testing could also help scientists collect samples more strategically during an outbreak to better monitor how the virus is spreading.
Next, the researchers are adapting SHINE to test for both avian and swine influenza strains. “With SARS-CoV-2 and now flu, we’ve shown that we can easily adapt SHINE to detect new or evolving viruses,” Arizti-Sanz says. “We’re excited to apply it to H5N1.”