Summary:
A new study by Weill Cornell Medicine researchers suggests that people with Crohn’s disease and joint inflammation have distinct gut microbiota, with the bacterium Mediterraneibacter gnavus identified as a potential biomarker for inflammation.
Takeaways:
- M. gnavus was found more frequently in Crohn’s patients with joint inflammation, suggesting its role as a biomarker.
- Different forms of joint inflammation (axial vs. peripheral spondyloarthritis) are associated with distinct gut microbiota compositions.
- Future research aims to identify immune-triggering bacterial components to develop targeted treatments for inflammation in Crohn’s disease.
People with Crohn’s disease and related joint inflammation linked to immune system dysfunction have distinct gut bacteria or microbiota, with the bacterium Mediterraneibacter gnavus being a potential biomarker, according to new study by Weill Cornell Medicine researchers.
The study, published in Gut Microbes, also demonstrated that the gut microbiota of people with Crohn’s and axial spondyloarthritis, which is joint inflammation of the spine and lower back, differs from individuals with Crohn’s and peripheral spondyloarthritis affecting other parts of the body like the knees, hips and shoulders.
“While joint inflammation is one of the most common extraintestinal manifestations of Crohn’s disease, clinicians don’t have a good handle on why this happens and how to treat it,” says the study’s senior author Dr. Randy Longman, MD, PhD, director of the Jill Roberts Center for Inflammatory Bowel Disease at Weill Cornell Medicine and NewYork-Presbyterian/Weill Cornell Medical Center and an associate professor of medicine at Weill Cornell Medicine.
Based on the new research, M. gnavus could serve as a biomarker for joint inflammation in Crohn’s disease patients, Longman says.
“The research also raises the possibility that there could be a causative link between the gut microbiota and immune cell responses that govern inflammation, but further investigation is needed,” he says.
Crohn’s Disease and Joint Inflammation
Crohn’s disease, an autoimmune disorder, affects more than half a million Americans and causes symptoms such as diarrhea, abdominal pain, weight loss and fatigue. Up to a third of patients may experience joint inflammation, although the reasons for this are not entirely clear, Longman says.
Normally, the gut lining acts as a barrier, keeping bacteria confined to the intestines. In people with Crohn’s disease and spondyloarthritis, this barrier may be compromised and lead to immune cell responses to specific gut bacteria associated with joint inflammation.
The Research Data
To explore which gut bacteria are linked to joint inflammation in Crohn’s disease, Longman and his colleagues analyzed deidentified stool samples from 106 people recruited from the Jill Roberts Center for Inflammatory Bowel Disease. This is one of the largest cohorts of patients that have been analyzed for this purpose, Longman says.
Samples were from 44 participants with Crohn’s disease without joint inflammation, 39 with Crohn’s disease and peripheral spondyloarthritis, 14 with Crohn’s and axial spondyloarthritis, and 9 healthy controls.
To gain a better understanding of the gut bacteria in these groups, Grace Maldarelli, MD, PhD, instructor in medicine in the Division of Infectious Diseases at Weill Cornell Medicine, took serum, the clear part of the blood, from study participants and incubated it with their stool samples. She then identified bacteria that were coated with a specific type of antibody, IgG. This type of antibody circulates in the blood, can recognize potential pathogens, and can drive inflammation. She sequenced these antibody-coated bacteria to identify which ones were associated with the different study subgroups.
Maldarelli found that IgG-coating of M. gnavus was observed in 33% of individuals with Crohn’s disease and peripheral spondyloarthritis and 29% with Crohn’s disease and axial spondyloarthritis, versus 11% in Crohn’s disease without inflammation and healthy controls.
The researchers also found that participants with Crohn’s disease without joint inflammation and Crohn’s disease with peripheral spondyloarthritis had distinct gut bacteria compared with healthy controls. In addition, the gut bacteria of individuals with Crohn’s disease with axial spondyloarthritis were distinct from Crohn’s disease with peripheral spondyloarthritis.
The level of IgG coating that the researchers saw in the peripheral blood also correlated with disease activity scores in patients with joint inflammation, Longman says.
Future Directions
M. gnavus has many epitopes, which are parts of the bacteria that the immune system can recognize and react to, Longman says. Future research may identify which epitope is responsible for causing an immune response so that scientists could target and alter this response as a potential treatment.
“Ultimately, I hope to figure out how to target or otherwise mitigate the effect of these bacteria on joint inflammation in patients with Crohn’s disease,” says Maldarelli, who is also an infectious disease specialist at NewYork-Presbyterian/Weill Cornell Medical Center.
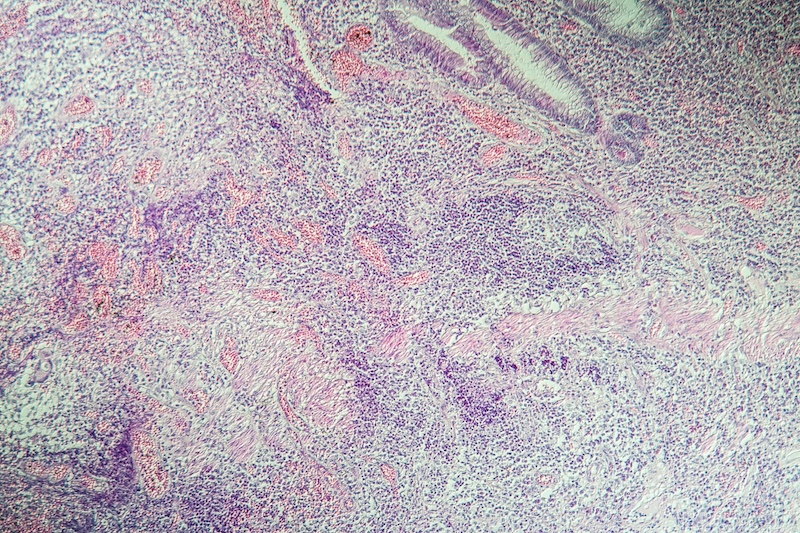
Featured Image: Norbert Dr. Lange | Dreamstime.com