While there is no gold standard TB diagnosis, WHO guidelines recommend the use of either the TST or IGRAs to test for latent tuberculosis infections.
By Jackie Weiss, PhD, and Maite Sabalza, PhD
Tuberculosis (TB) is an infectious disease caused by the bacillus Mycobacterium tuberculosis (Mtb) complex.1 The disease is spread through bacteria in airborne droplets expelled from patients who are sick with TB.2 While TB generally affects the lungs, it can disseminate throughout the body, especially in immunocompromised individuals.3
For simplicity, TB infections are generally classified as latent or active. However, TB exists on a spectrum ranging from containment of the infection to active disease,4 which is generally symptomatic and contagious.5 In some individuals infected with Mtb, the innate or adaptive immune response will eliminate the infection. If the immune system is unable to eliminate the infection, patients progress to latent TB infection (LTBI). In this stage, Mtb bacteria can remain dormant in the lungs, contained in a granuloma, or cluster of immune cells.4 If the granuloma is no longer able to contain the bacterial load, an individual will progress to subclinical or active TB. Patients with subclinical TB may not have symptoms, but patients who advance to active TB may have symptoms such as fever, weight loss, and cough.4 Notably, patients may ascend and descend through multiple stages over the course of the disease.4
In a minority of individuals, infection with Mtb can progress from an asymptomatic latent form to active disease.5 Reactivation of LTBI is responsible for most cases of active TB.5 Approximately 5-15% of patients with latent tuberculosis infection will progress to active TB,6 while the rest remain at risk of advancing to active TB during their lives.7 Therefore, it is important to detect and treat all stages of TB infection.
It has been estimated that approximately 25% of the world’s population has been infected with Mtb,8 but most of those infected will not develop disease.9 According to the World Health Organization (WHO), 10.6 million people developed active TB in 2021; most cases were localized to South-East Asia (45%), Africa (23%), and the Western Pacific (18%).1 In the United States, 8,300 cases of TB were reported in 2022.10 More than 80% of active TB cases in the U.S. are caused by reactivation of LTBI, highlighting the necessity of testing and treating those at higher risk. 11
TB remains a leading cause of death worldwide, responsible for 1.6 million deaths in 2021.1 Left untreated, the death rate for TB is approximately 50%.1 Fortunately, with proper treatment, about 85% of TB cases can be cured.1 The bacille Calmette-Guérin (BCG) vaccine, the only vaccine recommended to prevent TB, is often administered to infants and children in areas where TB is endemic. While the BCG vaccine protects against disseminated TB in children, it does not prevent Mtb infection or reactivation of latent tuberculosis infection.12
Why is it Important to Diagnose Latent Tuberculosis Infection?
By the year 2035, WHO’s End TB Strategy aims to reduce TB incidence by 90% and TB mortality by 95% compared to 2015. Accurate diagnosis of active TB, including drug susceptibility testing, is a key pillar of this strategy.13 However, an estimated 4 million cases of active TB were not diagnosed or officially reported in 2021. Because many cases of active TB result from reactivated LTBI, especially in low-incidence countries, it is critical to identify individuals with latent tuberculosis infection to prevent progression to active disease and further transmission.14,15
Making a Latent Tuberculosis Diagnosis
The detection of LTBI is based on measuring host memory T-cell response to Mtb. There are two methodologies used: 1) tuberculin skin test (TST); 2) interferon (IFN)-γ release assay (IGRA). Neither the TST nor IGRAs can distinguish between latent tuberculosis infection and active TB. Therefore, for detection of active TB, the WHO recommends microbiological methods rather than a TST or IGRA.16 Both TST and IGRAs are indirect tests for immune sensitization to Mtb. The main features of each assay are summarized in Table 1.
Table 1: Comparison of tests to diagnose latent tuberculosis infection.
| TST | IGRAs | |
| Testing type | Intradermal skin test | Blood test |
| Measuring | Type IV delayed hypersensitivity T-cell response | Interferon gamma T-cell response (IFN- γ) |
| Antigen used | Multiple | ESAT-6 and CFP-10 |
| Sensitivity | Poor sensitivity in immune-compromised | Good |
| Cross-reactivity with BCG vaccines | High | None |
| Cross-reactivity | MAC and most NTM species | M. kansasii, M. marinum and M. szulgai |
| Number of visits to the doctor | 2 visits | 1 visit |
| Cost | Low/medium | Medium |
The Tuberculin Skin Test
The tuberculin skin test (TST) is the first and most widely used diagnostic tool for latent tuberculosis infection, largely due to practitioners’ familiarity with the test and practicality in low-resource settings.16 The TST is a point-of-care (POC) test in which purified protein derivative (PPD), a mixture of mycobacterial antigens, is injected intradermally into the forearm. If the patient is infected, immune cells at the injection site will generate a delayed hypersensitivity reaction. The test result is determined by measuring the diameter of the induration at the injection site 48-72 hours after the initial injection.17
The TST has been used for over a century18 and has been widely characterized and studied. Since the TST does not require a lab space, this test is more feasible than other assays in resource limited settings.16 However, patients must return 48-72 hours after the PPD injection to have a valid test read and occasionally patients may not return, for example a study estimated that 20% of children did not return for TST.17,19 Therefore, the TST is of limited use in patients who will not return for a second visit. Additionally, PPD is a mixture of mycobacterial antigens that are not specific to TB.20 Consequently, cross-reaction and false positive results may arise in individuals infected with nontuberculous mycobacteria (NTM), or those who recently received a BCG vaccine.16 Finally, obtaining reliable results with the TST depends on rigorous standardization, training, supervision, and practice. Results are subject to providers’ interpretations; a previous study found that more than 90% of positive TST results were read as negative.21
Interferon Gamma Release Assays
Interferon gamma release assays (IGRAs) are two-step blood assays: First, stimulating blood cells (white blood cells) with Mtb antigens; followed by measuring interferon-gamma (IFN- γ) with an immunoassay.22 IFN-γ is usually released by white blood cells in most individuals who have been infected with Mtb. IGRAs require fresh whole blood, and the sample has to be processed in a clinical laboratory.
The U.S. Food and Drug Administration (FDA) has approved and made available four IGRAs in the United States, including T SPOT.TB (Oxford Immunotec LTD. [now Revvity]) based on ELISpot technology 23; two of the assays are based on ELISA.;25,26 and the newest one is based on chemiluminescence.27
For the T SPOT.TB test (the ELISPOT-based assay), the first step is the isolation of peripheral blood mononuclear cells (PBMCs) from fresh whole blood. Subsequently, the cells are washed, followed by quantification to establish a standardized cell count, and plated onto an ELISpot plate. Following that, the cells are stimulated with Mtb-specific antigens (ESAT-6 and CFP-10). The measurement of the IFN-y response is performed by quantifying the number of spots observed on the ELISpot plate. The result is reported as the number of interferon-gamma-producing T cells (spot-forming cells in antigen wells minus negative control wells).28 In ELISA—and chemiluminescence based assays, the cells are stimulated in the whole blood within the tubes coated with Mtb specific antigens (ESAT-6 and CFP-10). Subsequently, the plasma is separated and used to measure the IFN-γ response at the population level in an immunoassay that can be either an ELISA or CLIA.29,30 IGRAs are more specific than TSTs because the antigens utilized for cell stimulation do not cross-react with those used in the BCG vaccine or with non-tuberculous mycobacteria (NTM).31
Are There Guidelines for LTBI Diagnostics?
The WHO released updated global guidelines for the diagnosis of TB in 2022.16 In addition to global guidelines, there are country- and region-specific recommendations, as well as guidelines for specific populations at risk. 32,33 For example, TB screening is recommended for rheumatoid arthritis patients being considered for treatment with biological agents,34 PLWH,35 organ transplant candidates,36 kidney donors,37 and pregnant women at high risk of infection.38
There is no gold standard laboratory assay for TB diagnosis, but WHO guidelines recommend the use of either the TST or IGRAs to test for LTBI. The diagnostic guidelines acknowledge the benefits of the normalization step prior to cell stimulation required in the T-SPOT.TB test.39 Additionally, the WHO recommends the use of certain molecular tests for active Mtb infection as well as assessment of drug-resistance.16
In the United States, a task force, supported by the Centers for Disease Control and Prevention (CDC), American Thoracic Society (ATS), and the Infectious Disease Society of America (IDSA) updated recommendations for the detection of TB.40 The updated recommendations strongly recommended to perform an IGRA over a TST when latent tuberculosis infection testing is called for in people 5 years of age and older who are likely infected with Mtb, at a low or intermediate risk of disease progression, and have received the BCG vaccine or may not return to have a TST test read. Additionally, this update now recommends screening for LTBI in adult populations at increased risk.41
The Road to Eradication
More than a century has passed since TST was first used for LTBI diagnosis. Since then, it has seen widespread use, with IGRAs also playing a significant role. However, there are still many areas that have yet to be explored and improved. Additional studies are required to expand the existing data for the development of new clinical guidelines and public health recommendations to reduce TB incidence and mortality, particularly in populations at high risk. As guidelines and recommendations are evolving, it is crucial to actively monitor them and work together towards the shared goal of eliminating TB.
A major challenge is the lack of diagnostic tests that can differentiate between an active and latent TB infection and predict the progression from latent tuberculosis infection to active infection or clinical disease.42-44 More research is needed to assess the efficacy of existing assays for predicting the course of the disease, and new assays have to be developed to address this. Meanwhile, high-risk groups need to be screened for tuberculosis to stop the spread of the infection.
HIV infection is the greatest risk factor for TB infection; approximately one million people living with HIV (PLWH) are infected with TB each year.1 Additionally, TB is the leading cause of hospitalization and death of PLWH .45,46 TB-associated mortality is higher in PLWH compared to HIV-negative individuals due to accelerated disease progression and difficulties diagnosing TB in PLWH.47 Risk of severe disease and mortality is also high in children,48 who comprised 11% of TB cases worldwide in 2021.1 However, pediatric cases of TB are underdiagnosed, as radiological and clinical findings are often unspecific for TB in children. Additionally, it can be difficult to obtain sputum samples from children for microbiological testing.49
Pediatric patients and immunocompromised individuals, such as those with HIV or those on immunosuppressive therapy, are easy to identify and are considered as a TB high-risk population in guidelines for TB screening. However, there are additional individuals that could be considered high risk, including individuals living in poverty, those living in congregate settings, the homeless, the elderly, those experiencing elevated stress levels, excessive alcohol use, facing undernourishment, diabetes, smoking, or presenting with co-morbidities.1,50 It is also important to discuss that a weakened immune system can impact the performance of diagnostic tests that rely on an immune response to Mtb antigens. Therefore, normalizing the T-cell count before cell stimulation can help obtain accurate results in this vulnerable population.51
In summary, it is crucial to choose the appropriate test for each patient based on their specific circumstances. For instance, high-sensitivity assays are necessary for certain groups like the immunocompromised while the TST test lacks specificity in vaccinated individuals.
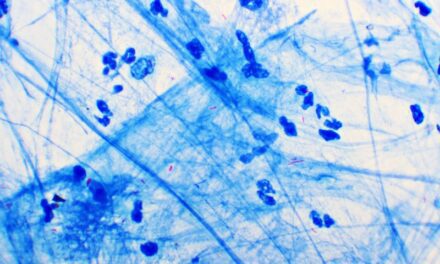
Featured Image: Latent tuberculosis infection can be diagnosed using TST or IGRAs. Image: EUROIMMUN US
ABOUT THE AUTHORS

Jackie Weiss, PhD is the Scientific Affairs Liaison at EUROIMMUN US (part of Revvity). Her role includes working with key opinion leaders on scientific collaborations, scientific writing, and supporting the team with commercial activities.

Maite Sabalza, PhD, is the Senior Scientific Affairs Manager at EUROIMMUN US (part of Revvity). Her academic background is in infectious diseases and diagnostics. In her role at EUROIMMUN US, she establishes relationships with key opinion leaders and supports the team with commercial activities including scientific collaborations, scientific marketing, and business development of diagnostics.
References
- WHO. Global tuberculosis report 2022. https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022. Published 2022. Accessed November 2, 2023.
- Migliori GB, Nardell E, Yedilbayev A, et al. Reducing tuberculosis transmission: a consensus document from the World Health Organization Regional Office for Europe. Eur Respir J. 2019;53(6).
- Hunter RL. The Pathogenesis of Tuberculosis: The Early Infiltrate of Post-primary (Adult Pulmonary) Tuberculosis: A Distinct Disease Entity. Front Immunol. 2018;9:2108.
- Pai M, Behr MA, Dowdy D, et al. Tuberculosis. Nat Rev Dis Primers. 2016;2:16076.
- Chee CBE, Reves R, Zhang Y, Belknap R. Latent tuberculosis infection: Opportunities and challenges. Respirology. 2018;23(10):893-900.
- Vynnycky E, Fine PE. The natural history of tuberculosis: the implications of age-dependent risks of disease and the role of reinfection. Epidemiol Infect. 1997;119(2):183-201.
- Horsburgh CR, Jr. Priorities for the treatment of latent tuberculosis infection in the United States. N Engl J Med. 2004;350(20):2060-2067.
- Houben RM, Dodd PJ. The Global Burden of Latent Tuberculosis Infection: A Re-estimation Using Mathematical Modelling. PLoS Med. 2016;13(10):e1002152.
- Emery JC, Richards AS, Dale KD, et al. Self-clearance of Mycobacterium tuberculosis infection: implications for lifetime risk and population at-risk of tuberculosis disease. Proc Biol Sci. 2021;288(1943):20201635.
- Schildknecht KR, Pratt RH, Feng PI, Price SF, Self JL. Tuberculosis – United States, 2022. MMWR Morb Mortal Wkly Rep. 2023;72(12):297-303.
- CDC. Latent TB Infection in the United States – Published Estimates. https://www.cdc.gov/tb/statistics/ltbi.htm. Published 2022. Accessed November 2, 2023.
- WHO. BCG vaccine. https://www.who.int/teams/health-product-policy-and-standards/standards-and-specifications/vaccines-quality/bcg Published 2023. Accessed November 2, 2023.
- WHO. The End TB Strategy. https://iris.who.int/bitstream/handle/10665/331326/WHO-HTM-TB-2015.19-eng.pdf?sequence=1. Published 2015. Accessed November 2, 2023.
- Shea KM, Kammerer JS, Winston CA, Navin TR, Horsburgh CR, Jr. Estimated rate of reactivation of latent tuberculosis infection in the United States, overall and by population subgroup. Am J Epidemiol. 2014;179(2):216-225.
- Lonnroth K, Migliori GB, Abubakar I, et al. Towards tuberculosis elimination: an action framework for low-incidence countries. Eur Respir J. 2015;45(4):928-952.
- WHO. WHO consolidated guidelines on tuberculosis. Module 3: diagnosis. Tests for tuberculosis infection. 2022.
- CDC. Tuberculin Skin Testing Fact Sheet. https://www.cdc.gov/tb/publications/factsheets/testing/skintesting.htm. Published 2020. Accessed November 2, 2023.
- von Pirquet C. Berlin klin Wochenschr. 1907(44):699-700.
- van der Heijden YF, Heerman WJ, McFadden S, Zhu Y, Patterson BL. Missed opportunities for tuberculosis screening in primary care. J Pediatr. 2015;166(5):1240-1245 e1241.
- Yang H, Kruh-Garcia NA, Dobos KM. Purified protein derivatives of tuberculin–past, present, and future. FEMS Immunol Med Microbiol. 2012;66(3):273-280.
- Kendig EL, Jr., Kirkpatrick BV, Carter WH, Hill FA, Caldwell K, Entwistle M. Underreading of the tuberculin skin test reaction. Chest. 1998;113(5):1175-1177.
- Yang Y, Wang H-J, Hu W-L, Bai G-N, Hua C-Z. Diagnostic Value of Interferon-Gamma Release Assays for Tuberculosis in the Immunocompromised Population. Diagnostics. 2022;12(2):453.
- FDA. Premarket Approval (PMA): T SPOT-TB TEST. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMA/pma.cfm?ID=320334. Published 2008. AccessedOctober 30, 2023.
- FDA. Premarket Approval (PMA): QUANTIFERON TB GOLD IN TUBE. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMA/pma.cfm?ID=335144. Published 2007. Accessed October 30, 2023.
- FDA. Premarket Approval (PMA): QuantiFERON – TB Gold Plus Test. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?ID=433767. Published 2019. Accessed Otcober 30,2023.
- Rudeeaneksin J, Srisungngam S, Klayut W, Bunchoo S, Bhakdeenuan P, Phetsuksiri B. QuantiFERON-TB Gold Plus and QuantiFERON-TB Gold In-tube assays for detecting latent tuberculosis infection in Thai healthcare workers. Rev Inst Med Trop Sao Paulo. 2023;65:e13.
- FDA. Premarket Approval (PMA): LIAISON QuantiFERON – TB Gold Plus. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?ID=433519. Published 2019. Accessed October 30, 2023.
- Kim TY, Chang HE, Lee SW, et al. A novel strategy for interpreting the T-SPOT.TB test results read by an ELISPOT plate imager. PLoS One. 2019;14(9):e0222920.
- Theel ES, Hilgart H, Breen-Lyles M, et al. Comparison of the QuantiFERON-TB Gold Plus and QuantiFERON-TB Gold In-Tube Interferon Gamma Release Assays in Patients at Risk for Tuberculosis and in Health Care Workers. J Clin Microbiol. 2018;56(7).
- Bisognin F, Lombardi G, Re MC, Dal Monte P. QuantiFERON-TB Gold Plus with Chemiluminescence Immunoassay: Do We Need a Higher Cutoff? J Clin Microbiol. 2020;58(10).
- Chen H, Nakagawa A, Takamori M, et al. Diagnostic accuracy of the interferon-gamma release assay in acquired immunodeficiency syndrome patients with suspected tuberculosis infection: a meta-analysis. Infection. 2022;50(3):597-606.
- Lewinsohn DM, Leonard MK, LoBue PA, et al. Official American Thoracic Society/Infectious Diseases Society of America/Centers for Disease Control and Prevention Clinical Practice Guidelines: Diagnosis of Tuberculosis in Adults and Children. Clin Infect Dis. 2017;64(2):e1-e33.
- ECDC. Handbook on tuberculosis laboratory diagnostic methods in the European Union. 2022.
- Singh JA, Saag KG, Bridges SL, Jr., et al. 2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis Rheumatol. 2016;68(1):1-26.
- Thompson MA, Horberg MA, Agwu AL, et al. Primary Care Guidance for Persons With Human Immunodeficiency Virus: 2020 Update by the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2021;73(11):e3572-e3605.
- AST. Mycobacterium Tuberculosis Infections in Solid Organ Transplantation
- OPTN. Guidance for Identifying Risk Factors for Mycobacterium tuberculosis (MTB) During Evaluation of Potential Living Kidney Donors.
- ACOG. Routine Tests During Pregnancy.
- WHO Guidelines Approved by the Guidelines Review Committee. In: WHO consolidated guidelines on tuberculosis: Module 3: diagnosis – rapid diagnostics for tuberculosis detection. Geneva: © World Health Organization 2021.; 2021.
- Lewinsohn DM, Leonard MK, LoBue PA, et al. Official American Thoracic Society/Infectious Diseases Society of America/Centers for Disease Control and Prevention Clinical Practice Guidelines: Diagnosis of Tuberculosis in Adults and Children. Clin Infect Dis. 2017;64(2):111-115.
- Mangione CM, Barry MJ, Nicholson WK, et al. Screening for Latent Tuberculosis Infection in Adults: US Preventive Services Task Force Recommendation Statement. Jama. 2023;329(17):1487-1494.
- Zellweger JP, Sotgiu G, Corradi M, Durando P. The diagnosis of latent tuberculosis infection (LTBI): currently available tests, future developments, and perspectives to eliminate tuberculosis (TB). Med Lav. 2020;111(3):170-183.
- Arinaminpathy N, Dowdy D. Understanding the incremental value of novel diagnostic tests for tuberculosis. Nature. 2015;528(7580):S60-S67.
- Abubakar I, Drobniewski F, Southern J, et al. Prognostic value of interferon-γ release assays and tuberculin skin test in predicting the development of active tuberculosis (UK PREDICT TB): a prospective cohort study. Lancet Infect Dis. 2018;18(10):1077-1087.
- Ford N, Shubber Z, Meintjes G, et al. Causes of hospital admission among people living with HIV worldwide: a systematic review and meta-analysis. Lancet HIV. 2015;2(10):e438-444.
- Ford N, Matteelli A, Shubber Z, et al. TB as a cause of hospitalization and in-hospital mortality among people living with HIV worldwide: a systematic review and meta-analysis. J Int AIDS Soc. 2016;19(1):20714.
- Meintjes G, Brust JCM, Nuttall J, Maartens G. Management of active tuberculosis in adults with HIV. Lancet HIV. 2019;6(7):e463-e474.
- Carvalho ACC, Kritski AL. What is the global burden of tuberculosis among children? Lancet Glob Health. 2022;10(2):e159-e160.
- Nicol MP, Zar HJ. Advances in the diagnosis of pulmonary tuberculosis in children. Paediatr Respir Rev. 2020;36:52-56.
- CDC. COVID-19 Vaccines for People Who Are Moderately or Severely Immunocompromised. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/immuno.html. Published 2023. Accessed November 1, 2023.
- Wong SH, Gao Q, Tsoi KK, et al. Effect of immunosuppressive therapy on interferon γ release assay for latent tuberculosis screening in patients with autoimmune diseases: a systematic review and meta-analysis. Thorax. 2016;71(1):64-72.