Progress and challenges on the way to a blood-based assay for PD-L1
By Michael A. Pritchett, DO, MPH; Jiaxin Niu, MD, PhD; Leisa Jackson; Hestia Mellert, PhD; and Gary A. Pestano, PhD
The programmed death-1/programmed death ligand-1 (PD-1/PD-L1) immune checkpoint represents a critical target for novel cancer immunotherapies. Antibody-based PD-1/PD-L1 inhibitors, which overcome tumor resistance to T-cell anticancer activity, have proven capable of generating durable responses and extending overall survival in patients with non-small cell lung cancer (NSCLC) or other cancers. However, their remarkable efficacy is highly selective, and limited to patients with specific but incompletely understood disease characteristics.
Factors governing PD-1/PD-L1 inhibitor susceptibility and resistance are likely multifold, and are a subject of intense research. Not only are anti-PD-1/PD-L1 immunotherapies extremely expensive, but they could also have serious side effects. Moreover, ineffective immunotherapy could lead to patients’ rapid deterioration, resulting in loss of opportunity to pursue any further therapy. Accurate patient selection is therefore imperative.
The current diagnostic method to predict anti-PD-1/PD-L1 immunotherapy responsiveness utilizes immunohistochemistry assays that detect the expression level of the PD-L1 protein in tumor tissue. However, the development pathway for the antibodies, methods, and interpretive standards is inconsistent. Diagnostic thresholds vary by tumor type and stage, prior therapeutic history, and the specific anti-PD-1/PD-L1 immunotherapy agent in use. With no universal reference standard, diagnostic interpretation can be inconsistent and subjective.
To address the current limitations of PD-L1 testing, several companies are working toward developing assays capable of detecting variable PD-L1 expression levels in peripheral blood, using a number of complementary approaches. While well grounded in theory, practical development of such tests has presented challenges of its own.
This article reviews the state of the art in PD-L1 diagnostic testing by immunohistochemistry, summarizes different approaches to developing a blood-based assay, and describes the design and objectives of a new clinical study designed to validate a plasma-based mRNA assay for guiding patient selection for anti-PD-1/PD-L1 immunotherapy.
Immunotherapies in Context
Non-small cell lung cancer (NSCLC) is the leading cause of cancer-related deaths worldwide.1In most patients, it lacks specific symptoms and cannot be detected until it is advanced and aggressively metastatic. The prognosis for patients with newly diagnosed NSCLC is grim, with an average 5-year survival rate of just 18%. When choosing the optimal therapeutic strategy, early detection and diagnosis are of the essence.
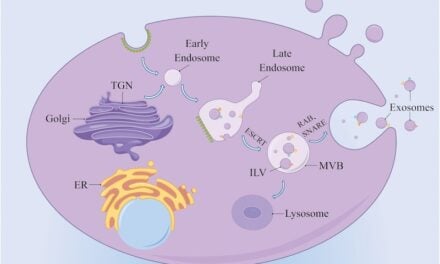
There are a growing number of systemic and targeted therapies for the disease, but patient responsiveness is highly variable and dependent on tumor biology and host immune characteristics. One mechanism for tumor resistance that has become an area of intense focus is the programmed death-1/programmed death ligand-1 (PD-1/PD-L1) checkpoint axis, which allows NSCLC and other cancers to evade the body’s system of acquired immunity by suppressing the activity of cytotoxic T cells (see “The PD-1/PD-L1 Checkpoint Blockade“).2 Novel cancer immunotherapies directed against PD-1 or PD-L1 have been developed to inhibit the immune checkpoint and overcome tumor resistance to cytotoxic T-cell activity. In some patients, the efficacy of these therapies has been remarkable, generating tumor regression with durable responses, and conferring clinically meaningful extension to overall survival.3
Despite its promise, the PD-1/PD-L1 checkpoint axis has also proven to be a challenging therapeutic target. While the response to anti-PD-1/PD-L1 immunotherapies can be robust, only one quarter to one half of patients experience clinical benefit.3Based on such heterogeneous response, it is clear that therapeutic efficacy is highly patient-specific. While clinical response appears to be associated with high PD-L1 expression within the tumor tissue, that relationship is non-binary, incompletely understood, and likely subject to the influence of other factors.
Anti-PD-1/PD-L1 immunotherapies are also very expensive. In the second-line setting, immunotherapy is expected to cost between $107,472 and $205,714 more per patient than standard chemotherapy, excluding the cost of any other drugs administered as part of a combination therapy.4
Tumor Tissue IHC: A Questionable Gold Standard?
The correlation between tumor PD-L1 overexpression and response to anti-PD-1/PD-L1 immunotherapies was established in clinical studies through the use of codeveloped immunohistochemistry (IHC) assays (Table 1).FDA has subsequently approved several such assays as companion or complementary diagnostics to guide patient selection. As a result, IHC testing is widely regarded as the current diagnostic ‘gold standard’ for clinical decisionmaking with respect to PD-1/PD-L1 immunotherapy.
However, IHC testing for PD-L1 expression is fraught with challenges—regardless of whether the test in use is an FDA-approved commercial diagnostic or a laboratory-developed test from an independent lab.3,6,7Some of the challenges are technical in nature and include the potential for tissue sampling error or inconsistencies; the variable quality of specific antibodies used to perform IHC; variability in pathologist interpretation; lack of standards for sample fixation and storage; and potential variations in results associated with proprietary assay components, solutions, and protocols.
With respect to the commercially available companion and complementary diagnostics, each assay relies on a different antibody for IHC detection, with thresholds and cutoffs that are not interchangeable, and are also dependent on cancer type and stage, history of prior therapy, and other factors stemming from the dynamic nature of PD-L1 expression and its presence in both healthy and diseased cells and tissue. This apples-to-oranges problem is significant enough that regulatory bodies have identified it as a potential patient safety concern. Not only could results from an incompatible test potentially be applied to the wrong therapeutic agent, but it has been estimated that current quantitative cutoffs may exclude as many as 10% to 20% of patients who could actually benefit from the drug in question.3
An attempt to harmonize the PD-L1 testing field, in fact, has been the focus of an unusually broad industry-academic-FDA partnership known as the Blueprint PD-L1 IHC Assay Comparison Project, which is designed to assess the analytical and clinical comparability of the four separate PD-L1 IHC assays used in clinical trials. Project findings published to date have confirmed that, although three of the four currently available IHC assays for PD-L1 display similar analytical performance, none were interchangeable for the purposes of classifying PD-1/PD-L1 immunotherapy responders.6,8 The effort is ongoing, with the addition of a fifth drug, avelumab, and its corresponding IHC test, which uses clone 73-10.9
Liquid Biopsy: An Alternative Approach
The history and challenges associated with PD-L1 IHC assays explains researchers’ active interest in adapting liquid biopsy techniques—whereby the presence of cancer biomarkers can be detected in blood—to determine an individual’s PD-L1 responder status. Based on findings for other biomarkers and in other cancer types, liquid biopsy from blood has a number of theoretical advantages over tissue IHC.
First, the interpretation of tissue IHC tests may lead to differences in results when compared to other methodologies. The discordance between IHC assays and nucleic acid-based assays, such as fluorescence in situ hybridization (FISH) assays, is a well-established phenomenon in cancer diagnostics. A 2002 study assessing 104 immunohistochemically positive (3+) breast carcinomas found that IHC and FISH test results for HER2 were not in agreement as much as 18% of the time.10A separate study of 697 cases from a single center found that 68% of the 19 discordant cases could be attributed to problems with the interpretation of IHC test results.11Although not strictly comparable to FISH, liquid biopsy techniques based on nucleic acid amplification assays have the potential to be more reproducibly quantitative than IHC tests because they are not subject to the common IHC weaknesses of analytic artifacts introduced by a combination of antibody-driven staining protocols, variations in detection methodology, or inconsistencies in scoring due to subjective interpretation.
Additionally, because liquid-biopsy samples are collected from blood and not from tissue, they confer virtually no patient risk to acquire, and they are less subject to confounding results caused by inaccurate sampling or other tissue-specific variables. Importantly, the simplicity and minimal invasiveness of blood draws means that patient samples can be assessed at multiple points during the treatment cycle, facilitating analysis over time of biomarker expression in response to treatment and during disease progression.
The overall average cost of liquid biopsy is also lower than IHC. A recent study comparing average total procedural costs of liquid biopsy compared to tissue biopsy from CT-guided fine needle aspiration or navigational bronchoscopy found that blood-based biopsies cost on average $7,404.05 less than navigational bronchoscopy and $3,250.52 less than CT-guided biopsies.12Treatment of complications associated with tissue biopsy procedures resulted in dramatically higher costs.
Taken together, the favorable qualities of liquid biopsies facilitate development of reference standards and tests that should be, at least in theory, more reliable, more reproducible, easier to interpret, and more useful over time than solid-tissue IHC.
A number of companies have taken on the challenge of developing assays to detect PD-L1 in blood in order to help guide treatment decisions regarding anti-PD-1/PD-L1 immunotherapies (Table 2).Four of those companies offer CLIA-certified, commercially available tests that use a variety of detection methods.
The PD-L1 test from BioCept, San Diego, is performed on circulating tumor cells, which are enriched using a proprietary, antibody-based, pan-circulating tumor cell (CTC) capture cocktail. The enriched cells are then stained with immunofluorescent antibodies for PD-L1 and other tumor-specific antigens, and measured by automated immunofluorescence.13
Like BioCept, Cynvenio, Westlake Village, Calif, uses a proprietary platform to capture and enrich CTCs from whole blood, with immunofluorescent detection of PD-L1 on the surface of cells performed on the resulting sample.14
Liquid Genomics, Torrance, Calif, offers a PD-L1 test as part of its LiquidGenomicsDx lung diagnostic panel. In contrast to the method used by BioCept and Cynvenio, the Liquid Genomics detection platform is based on the isolation of ctRNA from blood plasma, with subsequent reverse transcription and PD-L1-specific, quantitative PCR amplification.15
The PD-L1 expression test from Circulogene, Birmingham, Ala, detects cell-free RNA (cfRNA) using next-generation sequencing and a proprietary extraction-free, cell-free nucleic acid enrichment method. The company’s technique enables users to recover up to 100 times as much genetic material as industry-standard extraction methods, from as little as 20 mL of blood.16
Two other companies are currently developing liquid biopsy tests for PD-L1 with the aim of commercialization. One is Epic Sciences, San Diego, whose platform uses single-cell, automated digital pathology to characterize CTCs. After sample collection and lysis of red blood cells, nucleated cells are deposited onto a microscope slide and stained with immunofluorescent antibodies specific for tumor biomarkers. The slides are scanned at high resolution to map the location of individual cells, which can be analyzed by nucleic acid amplification or, in the case of PD-L1, by single-cell IHC.17

Figure 1. Laboratory workflow for RNA from blood. Prospectively collected whole blood samples are drawn into Streck RNA blood collection tubes for testing at the Biodesix CAP/CLIA-certified laboratory. Snap-frozen plasma samples stored at –80°C and shipped on dry ice are also feasible for RNA testing. Test samples for PD-L1 are accessioned and processed to isolate circulating RNA and generate cDNA using published methods. For ddPCR analysis, samples are processed using the Bio-Rad QX200 ddPCR system, and droplet counts are evaluated using QuantaSoft. Test results are generated in the final step of this 72-hour test process.20
The other company with a liquid biopsy test in development for PD-L1 is Biodesix, Boulder, Colo. The Biodesix platform is based on the use of droplet digital PCR (ddPCR), a technique for highly sensitive, quantitative, and reproducible amplification of circulating nucleic acids found in whole blood.18 Following sample collection and whole-blood fractionation, circulating RNA from the platelet-rich plasma is reverse transcribed, and the resulting cfDNA is partitioned into an oil emulsion that yields thousands of tiny droplets, each of which acts as an independent partition for amplification (Figure 1).19
Even for Liquid Biopsy, Challenges Remain
A review of recent data presented at meetings shows that, though promising, the development of liquid biopsy tests for PD-L1 has presented its own challenges. In particular, assessing PD-L1 in circulation is complicated by its expression in both immune and cancer cells. Proving concordance between liquid biopsy results and standard tissue IHC is therefore a difficult milestone for test validation.
At the 2017 AACR-NCI-EORTC International Conference on Molecular Targets and Cancer Therapeutics, Biodesix presented findings from a pilot effort to optimize its blood-based assay for PD-L1.19The study assessed assay feasibility using qPCR (Roche) and ddPCR (Bio-Rad) in tumor-derived cell lines, activated and resting immune cells, normal donor plasma, and NSCLC donor plasma (Figure 2). Concordance with IHC was also evaluated in a total of 16 tissue and blood samples that expressed cytokeratin 19 (CK19), which is a surrogate tumor biomarker for circulating RNA of epithelial origin.

Figure 2. Droplet digital polymerase chain reaction (ddPCR) validated by qPCR. PD-L1 mRNA levels were measured in cancer cell-lines NCI-H441, NCI-H226, HCC827, and SK-MES1 (blue); activated or resting immune cells (green); and normal healthy donor PEP (purple); by ddPCR (x-axis) and by qPCR (y-axis). The data demonstrate the high correlation (R2 = 0.984) between these two technologies.19
With respect to analytic performance, the Biodesix study found highly variable levels of plasma PD-L1 (from 2 to 1014 copies) in 52 of 57 NSCLC donor specimens evaluated using the ddPCR method (Figure 3).Five specimens were found to have fewer than 2 copies. The initial analysis of PD-L1 levels in blood (ddPCR) and tissue (IHC) at the 50% positive cut-off yielded poor concordance. Biodesix is exploring ways to evaluate whether concordance to a 1% cutoff value can provide actionable clinical information.
These promising initial findings demonstrate the technical feasibility of the PD-L1 circulating blood test as well as the possibility of identifying a meaningful, clinically relevant threshold for the assay. Consequently, Biodesix has combined with collaborators in its physician network, including FirstHealth Moore Regional Hospital and Pinehurst Medical Clinic, to validate the assay by analyzing prospectively collected, matched plasma and tissue samples from patients previously diagnosed with stage III or later NSCLC. The samples will be evaluated for PD-L1 in both tissue and plasma, and for the tumor cytokeratin biomarker in plasma.

Figure 3. PD-L1 expression in blood as measured by ddPCR. Large dynamic range of PD-L1 expression is detectable in prospectively collected blood samples. Fifty-seven prospectively collected whole blood specimens from donors with NSCLC were processed in the RNA development workflow in the Biodesix clinical laboratory. PD-L1 expression was analyzed using ddPCR and QuantaSoft.
The first objective of the study will be to assess the level of concordance between the results in plasma at 1% and 50% and IHC staining in the matched tissue samples. IHC staining will be conducted according to FDA-approved protocols using the PharmDx 22C3 antibody. The second objective of the study will be to assess PD-L1 mRNA transcript expression by ddPCR, and how that expression may correlate with immunotherapy performance measures that are currently in development. This latter objective may be conducted in order to compare PD-L1 expression levels to clinical outcomes. Importantly, the laboratory of PD-L1 testing expert Fred Hirsch at the University of Colorado Cancer Center will provide the centralized IHC testing in support of this study.
Conclusion
In certain NSCLC patients, PD-1/PD-L1-targeted immunotherapy can extend life in clinically meaningful ways. However, the marked heterogeneity of patient responses to the therapy indicates that there are specific but yet-to-be-understood characteristics that distinguish responders from nonresponders.
While the predictive value of other biomarkers—including indoleamine 2,3-dioxygenase (IDO), KRAS and its variants, mismatch repair deficiency/microsatellite instability (dMMR/MSI), programmed death-ligand 2 (PD-L2), and tumor mutational burden (TMB)—in tissue and in blood are still being explored, PD-L1 expression is likely to remain an important and essential part of the therapeutic decisionmaking toolkit. The development of validated tests for this biomarker has presented challenges at every step, but liquid biopsy holds promise to improve patient selection and outcomes for NSCLC.
Michael A. Pritchett, DO, MPH, is a pulmonologist at Pinehurst Medical Clinic and director of the Chest Center of the Carolinas at FirstHealth Moore Regional Hospital. Jiaxin Niu, MD, PhD, is the lead thoracic oncologist at Banner MD Anderson Cancer Center. Leisa Jackson is a senior research associate on the development team; Hestia Mellert, PhD, is director of development; and Gary A. Pestano, PhD, is vice president of development and operations, at Biodesix Inc. For further information, contact CLP chief editor Steve Halasey via [email protected].
References
- Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods, and major patterns in Globocan 2012. Int J Cancer. 2015;136(5):E359–386; doi: 10.1002/ijc.29210.
- Kim JM, Chen DS. Immune escape to PD-L1/PD-1 blockade: seven steps to success (or failure). Ann Oncol. 2016;27(8):1492–1504; doi: 10.1093/annonc/mdw217.
- Grigg C, Rizvi NA. PD-L1 biomarker testing for non-small cell lung cancer: truth or fiction. J Immunother Cancer. 2016;4:48; doi: 10.1186/s40425-016-0153-x.
- Treatment Options for Advanced Non-Small Cell Lung Cancer: Effectiveness, Value, and Value-Based Price Benchmarks: Final Evidence Report and Meeting Summary.Boston: Midwest Comparative Effectiveness Public Advisory Council, Institute for Clinical and Economic Review, 2016. Available at: https://icer-review.org/wp-content/uploads/2016/10/mwcepac_nsclc_final_evidence_report_meeting_summary_110116.pdf. Accessed March 5, 2018.
- Grady D. FDA approves first gene-altering leukemia treatment, costing $475,000. New York Times,August 30, 2017. Available at: www.nytimes.com/2017/08/30/health/gene-therapy-cancer.html. Accessed March 5, 2018.
- Hirsch FR, McElhinny A, Stanforth D, et al. PD-L1 immunohistochemistry assays for lung cancer: results from phase 1 of the Blueprint PD-L1 IHC assay comparison project. J Thorac Oncol. 2017;12(2):208–222; doi: 10.1016/j.jtho.2016.11.2228.
- Keeling P, Golebiewska E. The evolution of the PD-L1 testing market. Clinical Lab Products.2017;47(1):10–15. Available at: www.clpmag.com/2017/04/evolution-pd-l1-testing-market. Accessed January 14, 2017.
- Rimm DL, Han G, Taube JM, et al. A prospective, multiinstitutional, pathologist-based assessment of 4 immunohistochemistry assays for PD-L1 expression in non-small cell lung cancer. JAMA Oncol. 2017;3(8):1051–1058; doi: 10.1001/jamaoncol.2017.0013.
- Tsao M, Kerr K, Yatabe Y, Hirsch FR. Blueprint 2: PD-L1 immunohistochemistry comparability study in real-life, clinical samples [presentation abstract PL 03.03]. Paper presented at the world conference of the International Association for the Study of Lung Cancer, Yokohama, Japan, October 15–18, 2017. JThorac Oncol. 2017;12(11, Suppl 2):S1606; doi: 10.1016/j.jtho.2017.09.100.
- Paik S, Bryant J, Tan-Chiu E, et al. Real-world performance of HER2 testing: National Surgical Adjuvant Breast and Bowel Project experience. J Natl Cancer Inst. 2002;94(11):852–854.
- Grimm EE, Schmidt RA, Swanson PE, Dintzis SM, Allison KH. Achieving 95% cross-methodological concordance in HER2 testing: causes and implications of discordant cases. Am J Clin Pathol. 2010;134(2):284–292; doi: 10.1309/ajcpuqb18xzohhbj.
- Magee M, Arnaud A, Bowling M. Costs and outcomes comparison of tissue- and blood-based biopsies for the purpose of biomarker testing for advanced non-small cell lung cancer. Scientific presentation at the annual international meeting of the International Society for Pharmacoeconomics and Outcomes Research, Washington, DC, May 21–25, 2016.. Available at: www.ispor.org/research_pdfs/52/pdffiles/PCN57.pdf. Accessed March 5, 2018.
- Pircher T, Rimm D, Arnold L, Singh V. Validation of PD-L1 expression on circulating tumor cells in lung cancer [abstract P3.02c-067]. Poster presented at the world conference of the International Association for the Study of Lung Cancer, Vienna, December 4?7, 2016. J Thorac Oncol. 2017;12(1, Suppl):S1316–S1317; doi: 10.1016/j.jtho.2016.11.1862.
- PD-L1 Expression Test for Lung Cancer: LiquidBiopsy Blood Test [online]. Westlake Village, Calif: Cynvenio Biosystems, 2017. Available at: https://static1.squarespace.com/static/5967a3879f74565bc8914455/t/59af122bf5e231fa3dc04b6d/1504645675774/pd-l1-test-for-lung-cancer.pdf.Accessed March 5, 2018.
- Ishiba T, Usher JL, Elshimali Y, Vodala S, Sturdevant T, Dang M. Frequencies and expression levels of programmed death ligand 1 (PD-L1) in circulating tumor RNA (ctRNA) in various cancer types [abstract e23101]. Poster presented at the annual meeting of the American Society of Clinical Oncology, Chicago, June 3–7, 2016. J Clin Oncol. 2016;34(suppl):e23101; doi: 10.1200/jco.2016.34.15_suppl.e23101.
- Circulogene expands liquid biopsy testing capabilities, adds three cfRNA-based NSCLC tests supporting personalized treatment for lung cancer patients [press release, online]. Birmingham, Ala: Circulogene, 2017. Available at: http://circulogene.com/circulogene-expands-liquid-biopsy-testing-capabilities-adds-three-cfrna-based-nsclc-tests-supporting-personalized-treatment-for-lung-cancer-patients. Accessed March 5, 2018.
- Boffa DJ, Graf RP, Salazar MC, et al. Cellular expression of PD-L1 in the peripheral blood of lung cancer patients is associated with worse survival. Cancer Epidemiol Biomarkers Prev. 2017;26(7):1139–1145; doi: 10.1158/1055-9965.epi-17-0120.
- Hindson BJ, Ness KD, Masquelier DA, et al. High-throughput droplet digital PCR system for absolute quantitation of DNA copy number. Anal Chem. 2011;83(22):8604–8610; doi: 10.1021/ac202028g.
- Pritchett MA, Niu J, Jackson L, Mellert H, Pestano GA. Concordance of IHC and a new blood-based expression assay for the detection of PD-L1 in patients diagnosed with NSCLC [abstract A033]. Poster presented at the AACR-NCI-EORTC International Conference: Molecular Targets and Cancer Therapeutics, Philadelphia, October 26–30, 2017. Mol Can Ther. 2018;17(1, Suppl):abstract A033; doi: 10.1158/1535-7163.targ-17-ao33.
- Mellert HS, Alexander KE, Jackson LP, Pestano GA. A blood-based test for the detection of ROS1 and RET fusion transcripts from circulating ribonucleic acid using digital polymerase chain reaction. J Vis Exp. 2018;134:e57079; doi: 10.3791/57079.