In a recent study, researchers created a diagnostic test to identify functional intact sperm in infertile men that could change the treatment of male infertility and assisted reproductive technology.
“Male infertility is a recognized issue and deserves scientific and clinical attention,” says Andrei Drabovich, an assistant professor of laboratory medicine and pathology at the University of Alberta and corresponding author of the Molecular & Cellular Proteomics study.
One in every six couples trying to conceive experience infertility issues. In fact, about 10% of men in the United States are infertile. The most common cause of severe male infertility is a condition known as nonobstructive azoospermia, which results in the absence of sperm in the ejaculate due to poor sperm, or spermatozoa, development.
While assisted reproductive technology has improved exponentially over the past 50 years, according to Drabovich, extracting intact sperm from men with NOA can take up to 10 hours in the operating room and has varying rates of success.
“Sometimes surgeons can only extract a few intact spermatozoa during a surgery that takes many hours,” Drabovich says.
That’s why he set out to develop a noninvasive method to diagnose NOA and figure out if these men contain intact sperm that could fertilize an egg.
“Tests that show the presence or absence of intact spermatozoa in semen can give a good clue of the total numbers of spermatozoa in the patient,” Drabovich says. “If there are intact spermatozoa in the ejaculate that is a green light for urologists and the surgeon to go ahead with the surgery. However, it is an extreme challenge to find intact spermatozoa in a field of debris.”
Drabovich performed mass spectrometry on semen from men with normal fertility as well as infertile men with biopsy-confirmed obstructive azoospermia or NOA.
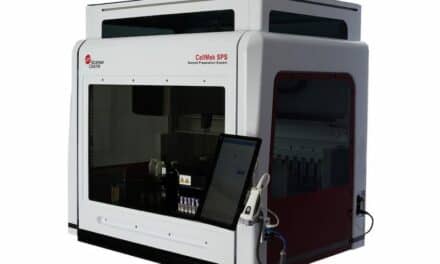
After analysis, his team identified two proteins, AKAP4 and ASPX, that are found in intact sperm in men with NOA. They showed that ASPX is located in the head of sperm while AKAPA4 is found in the tail using a method called imaging flow cytometry. During imaging flow cytometry, a machine takes images of individual cells. After running these samples, computational algorithms help the researchers mine the millions of images of cell debris and underdeveloped sperm to identify a few intact sperm cells.
Since the roles of AKAP4 and ASPX are not fully understood, Drabovich plans to investigate how they contribute to sperm function.
He also says that his work may lead to male birth control drugs in the future.
“We want to see if we can flip the story and try to work on male contraceptives,” Drabovich says. “If we know the function of the protein, we may be able to inhibit it to create a nonhormonal male contraceptive, which is a much desired type of drug at the moment.”