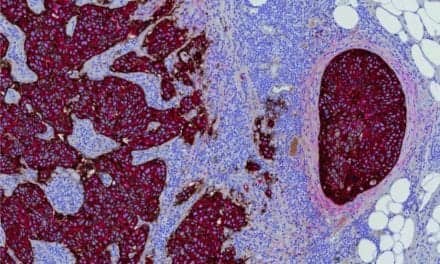
Coronary microvascular dysfunction (CMD), a condition in which the heart’s smallest arteries don’t dilate properly, has historically been difficult to diagnose due to tiny arteries not being visible on an angiogram. In fact, an estimated 50% of all angina cases are now attributed to CMD, with women accounting for most incidences. Yet, detecting CMD had, until now, remained elusive.
MedStar Heart & Vascular Institute became one of only a few programs in the nation to use the Coroventis CoroFlow Cardiovascular System. It is a software-based platform that, along with a special guidewire, can effectively measure the workings of the heart’s tiniest arteries, allowing physicians to confirm the cause of their patient’s unexplained chest pain.
CMD Diagnosis Case Study
Melanie McCauley of Fort Washington, Md., first experienced angina, or chest pain, at a bowling tournament. The tightness and pain in her chest, nausea, and sweating became so intense that she ended up in an ER. After a battery of tests, including an angiogram, which is an x-ray of the heart, found no blockages in her coronary arteries, she was sent home.
She returned to the ER several more times over the next few months. Each time, doctors assured her there was nothing wrong.
When her cardiologist referred her to MedStar Washington Hospital Center, which utilizes the Coroventis CoroFlow Cardiovascular System, Hayder Hashim, MD, determined a definitive diagnosis: coronary microvascular dysfunction. As a result, the heart doesn’t get enough oxygen-rich blood.
Effectively Diagnosing CMD
“For the first time, we now have the ability to correctly diagnose and then treat coronary microvascular dysfunction,” says Hashim, an interventional cardiologist at MedStar Washington Hospital Center. “As such, this innovative approach has the potential to help us prevent subsequent damage, improve quality of life, and give patients peace of mind.”
The assessment begins with an angiogram, followed by threading the guidewire through the left anterior descending artery. Once in place, the wire measures true blood flow and microvascular resistance, which the CoroFlow software then determines whether the heart’s smallest arteries are functioning properly.
“Patients with coronary microvascular dysfunction often feel dismissed by their doctor, like it’s ‘all in their head,’” says Brian Case, MD, an interventional cardiologist at MedStar Southern Maryland Hospital Center. “Yet, they know their pain is real, regardless of the lack of medical evidence. And that leaves them worried, unhappy, and even distrustful of the medical system. Even physicians are frustrated by their inability to provide optimal care for their patients. The CoroFlow platform should help both parties get the answers they seek.”
For McCauley, when Hashim told her she had coronary microvascular dysfunction, she felt immediate relief. “I started crying. I finally had a diagnosis and Dr. Hashim assured me that what I was experiencing was not in my head.”
After a diagnosis, CMD patients are returned to their referring physician for treatment and management. CMD is often treated with medications and/or lifestyle changes to control risk factors and reduce symptoms.
Doctors Hayder Hashim, Brian Case, and Itsik Ben-Dor have performed 140 of these procedures since its debut last year. They are also creating a CMD registry to follow patients long-term and further advance understanding of the disease.
Featured Image: Dr. Hayder Hashim uses the Coroflow platform in the Cath Lab. Photo: MedStar Washington Hospital Center