This is a companion article to the feature “Determining Molecular Response in Chronic Myeloid Leukemia.”
Droplet digital PCR (ddPCR) is rapidly becoming an invaluable tool in cancer treatment research. One such disease that especially benefits from ddPCR is non-small cell lung cancer (NSCLC), which accounts for 85% of all lung cancer cases, and has a 5% survival rate in metastatic cases.1
Tyrosine kinase inhibitors (TKIs) are an initial therapy option for patients with NSCLC. When patients develop resistance to TKIs, however, nearly half of these patients have the T790M mutation in the EGFR gene.1,2 This mutation can be found in cell-free tumor DNA (cfDNA) that can be obtained through liquid biopsies.2 After detecting the mutation during diagnosis, clinicians can use ddPCR to continue measuring the mutation throughout treatment. Such ongoing monitoring can improve treatment outcomes for patients because it helps doctors predict whether the patient will respond to TKIs.

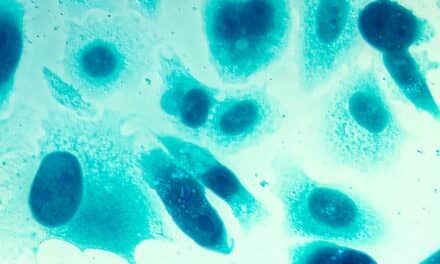
Figure 1. Liquid biopsy analysis by ddPCR (from left): researchers isolate plasma from a patient’s blood sample; ddPCR separates the plasma into individual droplets for PCR amplification and analysis; clinicians serially monitor the concentration of specific DNA mutations, such as T790M in non-small cell lung cancer, and adjust the patient’s treatment with tyrosine kinase inhibitors as needed.
While the current standard for analyzing cfDNA for the T790M mutation is quantitative PCR (qPCR), a study comparing qPCR to ddPCR has recently suggested that ddPCR may be a better choice.3 In their work, the researchers at Hermes Pardini Institute used qPCR and ddPCR to analyze cfDNA obtained from patient plasma through liquid biopsies (Figure 1).The goal was to establish preanalytical and analytical criteria for using ddPCR to measure T790M mutations levels in NSCLC liquid biopsy samples, and to determine the limit of detection and limit of quantification.
The ddPCR validation results showed high specificity (98.2%) and sensitivity (95.96%) and a low false-positive rate (0.2%).1All negative results found with ddPCR were concordant with negative results from patients tested by qPCR.1 Positive results between ddPCR and qPCR were concordant in 79% of cases. When testing was repeated for each sample, qPCR provided inconsistent results.1 According to the qPCR test manufacturer, this discrepancy was likely due to low levels of the T790M mutation in the blood (likely near or below the test’s limit of detection). On the other hand, ddPCR remained consistent across repeat testing of samples. This result suggests that ddPCR may be a more reliable method for analyzing cfDNA, according to the researchers.These findings will be used to establish best practices for ddPCR T790M analysis from NSCLC liquid biopsy samples.
The study was able to show that ddPCR could be an optimal method for detecting the T790M mutation because of its consistent results across all repeated tests. With an aggressive cancer such as NSCLC, consistent results are necessary to inform patient treatment. These preanalytical and analytical steps provide the foundation for ddPCR’s use in monitoring the T790M mutation in patients with NSCLC.
References
- Cirillo PDR, Marinho FLO, Machado CPFN, Freire MCM, Mateo EC, Zalis MG. Validation of preanalytical procedures of liquid biopsy samples for investigation of the EGFR-T790M mutation by ddPCR in NSCLC Brazilian patients [abstract B-294]. Poster presentation at the annual scientific meeting of the American Association for Clinical Chemistry, Chicago, July 29–August 2, 2018. Available at: https://files.abstractsonline.com/supt/2/4647/aacc18_instructionpage.html. Accessed October 29, 2018.
- Gedvilait? V, Schveigert D, Cic?nas S. Cell-free DNA in non-small cell lung cancer. Acta Med Litu. 2017;24(2):138–144; doi: 10.6001/actamedica.v24i2.3495.
- Bordi P, Del Re M, Danesi R, Tiseo M. Circulating DNA in diagnosis and monitoring EGFR gene mutations in advanced non-small cell lung cancer. Transl Lung Cancer Res. 2015;4(5):584–597; doi: 10.3978/j.issn.2218-6751.2015.08.09.