Droplet digital PCR can provide a more accurate assessment of low levels of BCR-ABL mRNA than quantitative real-time PCR
By Chinmay Sheth
One out of 526 people in the United States will be affected by chronic myeloid leukemia (CML) in their lifetime, and about 1,090 Americans die of the disease each year.1 CML was once considered a death sentence, but targeted drugs have transformed it into a manageable chronic disease with 5-year survival rates of 90%.2
To evaluate the disease status of patients with CML, clinicians use quantitative real-time PCR (qPCR) to periodically measure mRNA levels of the abnormal gene (BCR-ABL) whose expression causes CML. By monitoring BCR-ABL levels in response to therapy, physicians can measure disease burden and determine whether the patient’s disease is stable or progressing.
At very low levels of BCR-ABL, however, qPCR is not as sensitive as digital PCR (dPCR), potentially leading physicians to miss important insights that might alter the patient’s course of treatment. While qPCR can detect down to 1 copy of BCR-ABL for every 10,000 to 100,000 normal copies from patient samples, digital PCR can detect 1 copy of BCR-ABL for every 1 million to 10 million normal copies, offering a 2-log improvement in sensitivity.3–5 Such a heightened level of sensitivity may provide physicians with the ability to detect very small changes with greater accuracy, thereby enabling earlier intervention in patients with evidence of progressing disease.
Targeted Treatment Options for CML
CML is a cancer of myeloid progenitor cells in the bone marrow. When myeloid cells divide, pieces from chromosomes 9 and 22 can accidentally break off and switch places. One outcome of this randomly occurring ‘chromosomal translocation’ is that it leads parts of the BCR gene on chromosome 22 and the ABL gene on chromosome 9 to ‘fuse’ together, forming an abnormal fusion gene on chromosome 22 called BCR-ABL, also commonly known as the Philadelphia chromosome. This abnormal BCR-ABL gene encodes a tyrosine kinase that is always active, and results in uncontrolled production of white blood cells that can lead to symptoms such as increased fatigue, easier bleeding, more infections and, ultimately, death.
Tyrosine kinase inhibitors (TKIs) that target the BCR-ABL enzyme are one of the major standard therapy options for patients with CML. Scientists have consistently found that imatinib, a first-generation TKI, significantly improves the clinical outcomes of patients with CML: up to 97% of patients survive after 5 years.5 To keep the disease from progressing, however, most patients will need to take TKIs for the rest of their lives. Others will be able to discontinue treatment. Distinguishing between these two patient populations is one of the fundamental challenges facing the field.
Today, physicians are unable to predict with certainty which patients in remission will relapse based on BCR-ABL results measured using qPCR-based methods. Studies have documented relapse rates between 36% and 61% among patients who stop treatment based on qPCR results.6 To be safe, physicians typically continue to prescribe TKIs for all patients with CML for the rest of their lives.5
Lifelong reliance on TKI therapy, however, comes with its own difficulties. TKIs have a host of side effects that significantly affect quality of life. Common side effects include nausea, fatigue, and cramping; and more-serious side effects can include liver damage and congestive heart failure.7 Taking TKIs for an extended period of time can also be costly. A 2016 study estimated that the average annual cost for TKI drugs ranges between $59,000 and $76,000 per patient.8 Thus, a more sensitive and reliable disease monitoring method could lead to significant reductions in treatment costs and improved quality of life for these patients.
Assessing CML Progression
Physicians typically monitor the effectiveness of TKI therapy by measuring three types of responses:9
- Hematologic response. This measurement involves examining blood or bone marrow samples for signs of an unusually high white blood cell count.
- Cytogenetic response. This slightly more sensitive method is performed by taking a bone marrow biopsy and either using karyotyping to examine the sample for the presence of the Philadelphia chromosome, or using fluorescence in situ hybridization to tag BCR-ABL mRNAs with fluorescent probes.
- Molecular response.The most sensitive method for assessing TKI response is to measure the molecular response (MR). This test, which uses qPCR, detects and indirectly quantifies the levels of the BCR-ABL fusion gene in the blood relative to levels of the nonmutated gene, in most cases ABL.
Practice guidelines issued by the National Comprehensive Cancer Network and European Leukemia Net recommend that physicians monitor the molecular responses of patients with CML on TKI therapy every 3 months for 2 years after achieving a 1,000-fold (3-log) reduction in BCR-ABL levels relative to untreated CML (Table 1).5 This milestone is known as a ‘major molecular response’ and is assigned a molecular response score of 3 (‘MR3’). After 2 years of monitoring a patient who has attained MR3, physicians then monitor molecular response every 3 to 6 months until the patient relapses.
Patients can remain at or above MR3 indefinitely (increasing MR scores correspond to lower BCR-ABL concentration), but measuring BCR-ABL levels above MR3 can be challenging using qPCR.10–12 If a patient is experiencing drug resistance or disease progression, current qPCR techniques cannot precisely and reproducibly detect increases in BCR-ABL above MR3.3,4 Physicians may be able to identify these changes only much later, missing a crucial opportunity for early intervention.
Limitations of qPCR and Implications for BCR-ABLTesting
In qPCR, a sample is amplified through the real-time PCR instrument in a reaction mix that contains primers and fluorescent probes, and the concentration of the target DNA (ie, BCR-ABL) is measured over time. Quantitation of BCR-ABL levels requires comparison to a calibration curve using DNA standards of known concentration. Thus, BCR-ABL is only indirectly measured, which inherently introduces variability and subjectivity (eg, which DNA standards should be used for comparison?).
Many patients on TKI therapy reach a point called ‘minimal residual disease,’ where levels of BCR-ABL become undetectable using qPCR. A significant number of residual leukemic cells can remain in a patient considered to be ‘negative’ by qPCR, whose limit of detection can only reach 4–5 logs (that is, one BCR-ABL positive cell in 10,000 cells).5,13 The lack of sensitivity in these methods means that they cannot reveal with certainty whether a patient’s CML is in complete remission, leading physicians to keep them on lifelong TKI therapy.14,15
While qPCR is currently the recommended method for detecting BCR-ABL, lack of reproducibility is a common problem in clinical settings.13 For example, qPCR-based BCR-ABL tests can vary significantly across laboratories because of differences in specific reaction conditions, primer/probe selections, the reference genes used (ABL, BCR, and others), the DNA standards used for the calibration curves, and the qPCR platforms used for detection.10–12 Even with the development of a standardized reporting system called the percent International Scale (%IS), which attempts to harmonize protocols across labs, a study across 38 laboratories found that only 58% of laboratory methods achieved an average BCR-ABL difference of ±1.2-fold with respect to a reference method in a centralized laboratory.12
In order for physicians to be able to discontinue TKI treatment for patients with CML who have achieved complete remission, thereby improving their quality of life, they need to be able to detect minimal residual disease with greater certainty.
Monitoring CML with ddPCR-Based Methods
A new test for monitoring BCR-ABL overcomes the limitations of qPCR by employing a novel approach called droplet digital PCR (ddPCR). The underlying chemistry of qPCR- and ddPCR-based methods is similar: both techniques employ standard PCR reagents, oligonucleotide primers, and fluorescent probes to amplify specific DNA sequences (Table 2).
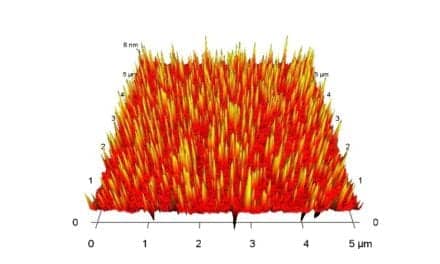
Unlike qPCR, however, ddPCR separates each sample into thousands of nanoliter-sized droplets in which PCR reactions are performed. The target DNA in each droplet is amplified such that only the droplets containing the target DNA fluoresce. These droplets are then read as either ‘positive’ or ‘negative’ based on the presence or absence of a fluorescent signal. The number and fraction of positive droplets is then used to calculate the absolute number of starting DNA copies. Thus, unlike qPCR, ddPCR provides direct quantification of target nucleic acids, improving the precision and reproducibility of the test. Droplet digital PCR can measure BCR-ABL concentrations to within ±10%.16

Figure 1. Droplet digital PCR increases the signal-to-noise ratio to the level needed to detect rare DNA sequences such as BCR-ABL gene fusions. From left: the sample is partitioned into 20,000 nanoliter-sized droplets; each droplet undergoes PCR amplification to endpoint, and droplets that contain the target DNA fluoresce; positive droplets are counted to enable absolute and precise quantification of the target sequence.
Partitioning the sample allows ddPCR to detect very low abundance targets (Figure 1). Since target DNA is present in varying abundance in different droplets, the competition for primers and probes is reduced, giving the PCR reaction a better chance at detection.17 According to one study, ddPCR provided a more than 2-log increase in sensitivity for detecting BCR-ABL, when compared to the standard qPCR assay.4 The advantages in precision and sensitivity offered by ddPCR can be used to closely monitor even small changes in BCR-ABL levels, particularly when the levels go above MR3.4 In theory, if disease progression is detected sooner by ddPCR, physicians can alter treatment, thus improving clinical outcomes.
A ddPCR-Based CML Monitoring Test
The ddPCR-based CML test mentioned above was recently CE marked, and is now in use as a clinical monitoring test in Europe, Hong Kong, and New Zealand. Developed by Bio-Rad Laboratories, Hercules, Calif, the QXDx BCR-ABL %IS test is also under review by FDA, and is the first ddPCR-based molecular diagnostic for monitoring CML treatment (Figure 2).
The QXDx BCR-ABL %IS kit enables absolute quantification of BCR-ABL copies in blood samples, eliminating the need for standard calibration curves, and minimizes variability between samples.4 The test can also quantify BCR-ABL transcripts at levels far beyond the currently established MR3 clinical cutoff value: it can detect molecular response values up to 4.7 and 5.0 in 2-well and 4-well test formats, respectively. The MR5 level corresponds to 0.001 %IS value, or one BCR-ABL copy in 100,000 ABL copies.
The readout of the QXDx BCR-ABL %IS kit reports directly in both %IS and MR values without the need to use laboratory-specific conversions, contributing to efforts to standardize test results and the clinical management of patients with CML.
The QXDx BCR-ABL test’s high sensitivity and ddPCR technology’s inherent precision may help physicians more confidently determine BCR-ABL levels associated with complete remission in patients with CML.
One of the limitations of the QXDx BCR-ABL %IS kit is that it does not detect and quantify every variant of BCR-ABL. The kit is designed to measure two of the most common varieties of the BCR-ABL fusion transcript (types e13a2 and e14a2). While these transcripts comprise more than 97% of cases, the kit cannot be used to monitor other rare BCR-ABL fusion transcripts, including e1a2 (which encodes p190 BCR-ABL) and e19a2 (which encodes p230 BCR-ABL), nor can it measure transcripts associated with other forms of leukemia.18
The QXDx BCR-ABL %IS kit also does not differentiate between the two transcript types it’s designed to detect, which may have different diagnostic implications. The test is only intended to measure treatment response in patients who have already tested positive for the Philadelphia chromosome; it is not designed to diagnose CML.
Future Developments
In order to gain acceptance in the clinic, ddPCR will need to be validated alongside current qPCR methods. For instance, the Life after Stopping TKI study—scheduled for completion in September 2019—is a prospective trial designed to determine the percentage of patients with an MR greater than 4 who experience molecular recurrence after discontinuing TKI therapy.19 The trial will also use ddPCR to concurrently monitor BCR-ABL levels in these patients, providing an important clinical comparison between the two methods.20 This study, the largest of its kind, is expected to lead to better criteria for patient selection in future TKI discontinuation studies.
The QXDx BCR-ABL %IS kit represents one of many potential applications for ddPCR. Beyond CML, ddPCR-based tests may also be able to monitor treatment responses for other forms of leukemia and other types of cancer, including bladder and lung cancers as well as melanoma (see “Creating More Accurate Measurements of NSCLC Treatment Response”).
It has been 20 years since the use of TKIs revolutionized care for CML patients, making this previously deadly disease into a manageable condition. Now ddPCR has the potential to significantly improve the ways that physicians care for patients who are treated with TKIs.
Chinmay Sheth is marketing product manager for the clinical diagnostics portfolio of the digital biology group at Bio-Rad Laboratories. For further information, contact CLP chief editor Steve Halasey via [email protected].
References
- Key Statistics for Chronic Myeloid Leukemia [online]. Atlanta, Ga: American Cancer Society, 2018. Available at: https://bit.ly/2w6t0gD. Accessed September 10, 2018.
- Druker BJ, Guilhot F, O’Brien SG, et al. Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med. 2006;355(23):2408–2417; doi: 10.1056/NEJMoa062867.
- Goh HG, Lin M, Fukushima T, et al. Sensitive quantitation of minimal residual disease in chronic myeloid leukemia using nanofluidic digital polymerase chain reaction assay. Leuk Lymphoma. 2011;52(5):896–904; doi: 10.3109/10428194.2011.555569.
- Jennings LJ, George D, Czech J, Yu M, Joseph L. Detection and quantification of BCR-ABL 1 fusion transcripts by droplet digital PCR. J Mol Diagn. 2014;16(2):174–179; doi: 10.1016/j.jmoldx.2013.10.007.
- Morley A. Quantifying leukemia. N Engl J Med. 1998;339(9):627–629; doi: 10.1056/NEJM199808273390911.
- Baccarani M, Deininger MW, Rosti G, et al. European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Blood. 2013;122(6):872–884; doi: 10.1182/blood-2013-05-501569.
- Mori S, Vagge E, le Coutre P, et al. Age and dPCR can predict relapse in CML patients who discontinued imatinib: the ISAV study. Am J Hematol. 2015;90(10):910–914; doi: 10.1002/ajh.24120.
- Side Effects of Tyrosine Kinase Inhibitor (TKI) Therapy [online]. Rye Brook, NY: Leukemia and Lymphoma Society, 2018. Available at: www.lls.org/leukemia/chronic-myeloid-leukemia/treatment/side-effects. Accessed September 14, 2018.
- Padula WV, Larson RA, Dusetzina SB, et al. Cost-effectiveness of tyrosine kinase inhibitor treatment strategies for chronic myeloid leukemia in chronic phase after generic entry of imatinib in the United States. J Natl Cancer Inst. 2016;108(7); doi: 10.1093/jnci/djw003.
- Soverini S, De Benedittis C, Mancini M, Martinelli G. Best practices in chronic myeloid leukemia monitoring and management. Oncologist. 2016;21(5):626–633; doi: 10.1634/theoncologist.2015-0337.
- Müller MC, Erben P, Saglio G, et al. Harmonization of BCR-ABL mRNA quantification using a uniform multifunctional control plasmid in 37 international laboratories. Leukemia. 2008;22(1):96–102; doi: 10.1038/sj.leu.2404983.
- Zhang T, Grenier S, Nwachukwu B, Wei C, Lipton JH, Kamel-Reid S. Interlaboratory comparison of chronic myeloid leukemia minimal residual disease monitoring. J Mol Diagn. 2007;9(4):421–430; doi: 10.2353/jmoldx.2007.060134.
- Branford S, Fletcher L, Cross NCP, et al. Desirable performance characteristics for BCR-ABL measurement on an international reporting scale to allow consistent interpretation of individual patient response and comparison of response rates between clinical trials. Blood. 2008;112(8):3330–3338; doi: 10.1182/blood-2008-04-150680.
- Branford S, Seymour JF, Grigg A, et al. BCR-ABL messenger RNA levels continue to decline in patients with chronic phase chronic myeloid leukemia treated with imatinib for more than 5 years and approximately half of all first-line treated patients have stable undetectable BCR-ABL using strict sensitivity criteria. Clin Cancer Res. 2007;13(23):7080–7085.
- Sanders R, Mason DJ, Foy CA, Huggett JF. Considerations for accurate gene expression measurement by reverse transcription quantitative PCR when analyzing clinical samples. Anal Bioanal Chem. 2014;406(26):6471–6483; doi: 10.1007/s00216-014-7857-x.
- Hindson BJ, Ness KD, Masquelier DA, et al. High-throughput droplet digital PCR system for absolute quantification DNA copy number. Anal Chem. 2011;83(22):8604–8610; doi: 10.1021/ac202028g.
- Hughes T, Deininger M, Hochhaus A, et al. Monitoring CML patients responding to treatment with tyrosine kinase inhibitors: review and recommendations for harmonizing current methodology for detecting BCR-ABL transcripts and kinase domain mutations and for expressing results. Blood. 2006;108(1):28–37; doi: 10.1182/blood-2006-01-0092.
- Huggett JF, Cowen S, Foy CA. Considerations for digital PCR as an accurate molecular diagnostic tool. Clin Chem. 2015;61(1):79–88; doi: 10.1373/clinchem.2014.221366.
- Atallah E, Schiffer CA, Weinfurt KP, et al. Design and rationale for the life after stopping tyrosine kinase inhibitors (LAST) study, a prospective, single group longitudinal study in patients with chronic myeloid leukemia. BMC Cancer. 2018;18(1):359; doi: 10.1186/s12885-018-4273-1.
- Cross NCP, White HE, Colomer D, et al. Laboratory recommendations for scoring deep molecular responses following treatment for chronic myeloid leukemia. Leukemia. 2015;29(5):999–1003; doi: 10.1038/leu.2015.29.