Summary
Rapid immunoassays are increasingly used in emergency diagnostics, particularly for conditions such as cardiac events, sepsis, and respiratory issues. Their value lies in providing fast results, crucial in emergency settings. However, a balance must be struck between speed and analytical sensitivity. This article explores where these assays are gaining traction and examines the opinions of laboratorians in emergency departments.
Key Takeaways
- Rapid immunoassays are becoming more prevalent in emergency departments for conditions like cardiac events and sepsis.
- While fast results are crucial in emergencies, they often come with trade-offs in analytical sensitivity.
- New techniques and technologies continue to evolve, aiming to improve both the speed and accuracy of these tests.
- Regulatory considerations remain important as rapid testing becomes more widespread.
- Perspectives from laboratory technicians highlight both the benefits and challenges of adopting rapid immunoassays.
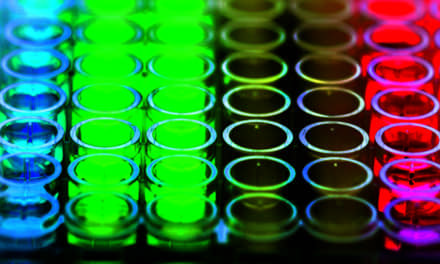
Rapid immunoassays have emerged as a valuable tool for providing quick information that can be crucial in life-threatening situations. Traditionally, the use of these assays has seen a focus on cardiac markers, respiratory conditions, and sepsis, where time is of the essence. With the pressure to deliver quick results, laboratories are faced with the challenge of balancing speed with the necessary accuracy and sensitivity.
Growing Applications in Emergency Medicine
Emergency departments have long relied on rapid immunoassays for detecting cardiac markers such as troponin, a protein released when the heart muscle is damaged. As of recent updates, institutions like the American College of Cardiology acknowledge the diagnostic value of these assays in quickly ruling out myocardial infarction. This rapid turnaround is immensely beneficial as it helps to triage patients and guide further testing or interventions.
The utility of rapid tests is not confined to cardiac conditions. In cases of suspected sepsis, timely identification is critical. Sepsis remains one of the leading causes of mortality in hospitals worldwide. Rapid immunoassays aimed at detecting biomarkers indicative of sepsis allow physicians and clinical teams to act swiftly.
Another area seeing uptake is respiratory panels, especially during periods of high incidence of flu and other respiratory viruses. Panels capable of detecting multiple pathogens from a single sample enable quick decision-making, crucial in managing outbreaks effectively and efficiently.
Balancing Speed with Sensitivity
While rapid immunoassays offer advantages in terms of time, a notable challenge lies in ensuring reliable results. Speed often comes at the cost of sensitivity and specificity, factors that are integral to accurate diagnostics. As tests aim to deliver faster results, laboratorians are tasked with evaluating these trade-offs.
Efforts to refine these assays have led to incremental improvements. For example, advances in technology have increased the sensitivity of assays, reducing false-negative results. Techniques such as chemiluminescence and advanced enzymatic labels are among the latest advancements enhancing test performance.
Regulatory scrutiny also plays a significant role in ensuring quality. Agencies such as the FDA continue to evaluate and approve rapid immunoassays, considering both their speed and efficacy. This regulatory landscape remains dynamic, requiring laboratorians to keep abreast of updates that affect assay implementation and utility.
As rapid immunoassays become more entrenched in clinical settings, the need for continuous education and training becomes evident. Laboratories must invest in ensuring technicians can adeptly handle the equipment and interpret results accurately, underscoring the importance of incorporating best practices into regular workflow.
Laboratorians in emergency departments acknowledge the dual nature of rapid immunoassays. While offering clear benefits in urgency, these tests must be balanced with a grasp of their limitations to avoid compromising diagnostic integrity. Open channels between laboratory teams and emergency physicians can aid in refining testing strategies that maximize both speed and accuracy, thus enhancing patient outcomes.
ID 184315110 © Lutfi Hanafi | Dreamstime.com