Two FDA-approved molecular testing platforms are leading to better targeted treatments for this common infection.
By Oluwatosin Goje, MD, MSCR
Two FDA-approved in vitro diagnostic (IVD) molecular testing platforms that use nucleic acid amplification testing (NAAT) to detect vaginitis pathogens can help advance how clinicians diagnose and treat this leading health problem among women.1,2
These assays are intended for the diagnosis of pathogens in women with signs and symptoms of vaginitis so that healthcare providers will no longer need to rely on subjective traditional diagnostic testing methods. NAATs, and other molecular approaches to vaginitis testing, deliver increased testing accuracy compared with traditional methods.3 Vaginal swabs, which can be collected by healthcare providers or self-collected by patients, are run on automated platforms that interrogate the samples for multiple different pathogens and minimize the risk for sample contamination. Minimal training is needed to implement NAAT testing for vaginitis in the clinical laboratory, with results that are reproducible and interpretations that are objective. NAATs streamline delivery of reliable vaginitis diagnoses that alongside clinical symptoms can guide effective treatments targeted to the appropriate pathogen, leading to better health outcomes for women.
Vaginitis Pathogens
Most women experience an episode of vaginitis at least once in their lifetime.4 The infection is the most common reason women visit obstetrician/gynecology specialists and other healthcare providers,5 and symptomatic vaginitis accounts for millions of clinical visits annually.6 Three different types of pathogens are most often associated with the infections:
• Bacterial vaginosis (BV) occurs in 40% to 50% of vaginitis cases.4 Bacterial species frequently detected include Gardnerella vaginalis, Atopobium vaginae, Megasphaera types, Leptotrichia amnionii, Sneathia sanguinegens, Porphyromonas asaccharolytica, a bacterium related to Eggerthella hongkongensis, and
bacteria related to Prevotella spp.3 In the United States the prevalence of BV is 21 million cases.7
• Fungal infections are a second common vaginitis pathogen mainly caused by Vulvovaginal candidiasis (VVC), which accounts for up to 20% to 25% of vaginitis cases. The most common fungal pathogen is C. albicans, appearing in approximately 90% of vaginitis cases, with Candida glabrata detected in most of the remaining cases.8 Approximately 75% of women will have a VVC infection in their lifetime; nearly 50% will have two or more VVC episodes.9
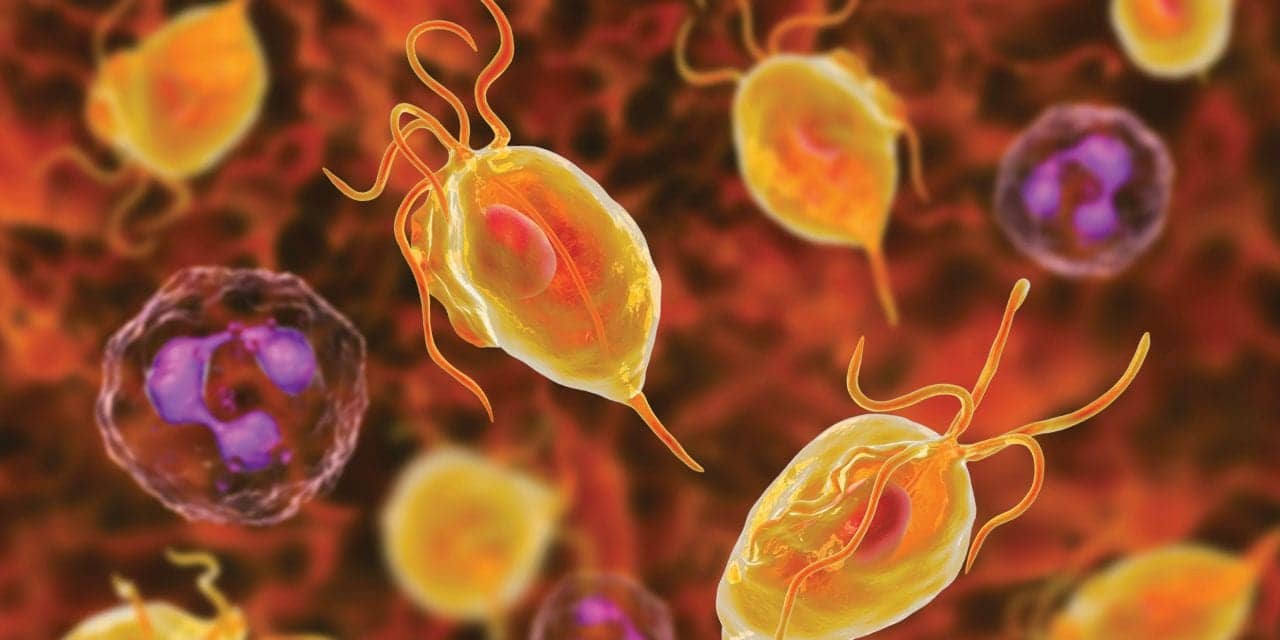
• A parasitic infection, trichomoniasis (TV), is also a common source of vaginitis, caused most frequently by the species Trichomonas vaginalis, which occurs in 15% to 20% of cases.4 An estimated 3 million cases of Trichomonas vaginalis occur each year in the United States.
The type of pathogen, its intrinsic virulence, and the relative dominance of the various recovered bacteria affect the characteristics of vaginitis infections.3 Diagnostic complexity is exacerbated when multiple pathogens are present, especially when more than one type contributes to vaginitis symptoms.10,11 Approximately 20% to 30% of women with BV are coinfected by Candida spp., and the coexistence of bacterial pathogens and Trichomonas vaginalis is also often reported (coinfection rates of 60–80%).6,12,13 Interactions between pathogens during an infection may influence the antimicrobial susceptibility of both organisms, which has implications for treatment decisions and medication efficacy.6
Limits of Traditional Testing
Healthcare providers traditionally diagnose vaginitis by considering the combination of symptoms, physical examination, Amsel criteria (pH of vaginal fluid, evaluation of discharge, microscopy, whiff test), and the Gram stain by standard methods.14 When combined with symptoms and physical examination, and compared with a DNA probe standard, these tests have a sensitivity and specificity rates of 81% and 70%, respectively, for BV; 84% and 85% for VVC; and 85% and 100% for TV.14 Amsel criteria compared with NAAT platforms have been reported with even lower sensitivities (75.6% vs 92.7%, respectively).12,15
Together these performance results indicate false negative test reporting is more common with traditional methods than molecular-based assays, which translates to either missed or misdiagnosed infections.
Clinicians often have difficulty identifying more than one pathogen responsible for vaginitis.3 Some may not have access to specific diagnostic tools, such as a microscope, in the clinic setting, or they may not adhere to the strict diagnostic criteria of clinical indicator tests.3 In a study designed to assess how women with vaginal discharge syndromes were being evaluated in community practice settings and to assess the appropriateness of the treatments prescribed for BV, VVC, and TV, investigators found that 42% of women having vaginitis symptoms received inappropriate treatment.16 This study suggested that Centers for Disease Control and Prevention-recommended point-of-care testing—such as assessment of vaginal pH, microscopic examination of vaginal fluid, or the whiff test—is actually not performed and prescriptions are often instead based on symptom presentation and other empiric observations.
Harms of Inadequate Testing
Untreated or inappropriately treated vaginitis may lead to pelvic inflammatory disease3 and its sequalae of infertility.17 Other fertility-related adverse outcomes of vaginitis include preterm births, recurrent abortions, and stillbirths.18 Persistent vaginitis also increases the risk of acquiring human immunodeficiency virus and other sexually transmitted infections.18
Inaccurate or absent vaginitis test results, and reliance only on symptom assessment, are problematic for treatment efficacy as they deprive patients of effective treatments or drive prescriptions for the wrong medications.6 Up to 15% of vaginitis patients fail to respond to initial antimicrobial therapy, suggesting that they had been misdiagnosed.18 Up to 80% of patients who respond to treatment for vaginitis have recurrence of infection symptoms and need repeat administration of antibiotics, suggesting that at least one symptom-causing pathogen was undetected.
The Hillier study demonstrated that overtreatment of noninfected women (false-positive misdiagnosis) also has adverse consequences.16 Women without infections who received treatment based on inaccurate or insufficient diagnostic evidence were more likely to have recurrent visits to the clinic within 90 days of initial visit.
Experts have raised awareness of how essential correct diagnoses are to prevent both under- and overdiagnosis of vaginitis and the negative consequences of inappropriate treatment.19 At a 2016 meeting of women’s health leaders from across the United States, experts concluded that diagnostic accuracy for vaginitis must be improved through better, faster diagnostic tools.20
Recently updated American College of Obstetricians and Gynecologists (ACOG) Practice Guidelines recommend NAAT be used for diagnosis of trichomoniasis and suggest that these methods can also be used as an alternative to the recommended Amsel and Nugent criteria tests for BV.5
FDA-Approved IVD Platforms for Vaginitis
The Hologic Aptima BV and Aptima CV/TV vaginitis testing platforms were FDA-approved for IVD in 2019.1,15 The NAAT assays are run on Hologic’s Panther platform. Among pathogens tested for by the Aptima system are the bacterium Lactobacillus species (L. gasseri, L.crispatus, and L. jensenii), G. vaginalis, and A. vaginae; fungal species in the Candida group (C. albicans, C.a dubliniensis, C. parapsilosis, and C. tropicalis) and C. glabrata; and the T. vaginalis parasite.
As part of the FDA requirements for assay performance validation, a multicenter cross-sectional diagnostic-accuracy study was conducted to evaluate the clinical performance of the investigational Aptima BV and Aptima CV/TV NAAT assays.15 The clinical trial, which evaluated performance of both assays, enrolled 1,519 subjects across 21 geographically and ethnically diverse sites in the United States. Subjects in the studies were 14 years of age or older and had symptoms of vaginitis. Multiple vaginal-swab samples were collected in the clinic from each patient during clinical visits, and results were compared to Nugent (plus Amsel for intermediate Nugent) scores for BV, to Candida cultures and DNA sequencing for CV, and to a composite of NAAT and culture for T. vaginalis.
Overall, infection rates identified by the reference methods and the investigational assays were similar, and similar infection rates were obtained for the investigational assays between clinician- and patient-collected swabs. Approximately 50% of infections were BV, approximately 30% were VVC, and 10% were TV. Coinfection rates by two or more organisms were 20% by reference testing and approximately 25% by investigational testing. Overall sensitivity estimates for the Aptima tests in clinician-collected samples were greater than or equal to 90% for BV, the Candida group, and for TV (Table 1). Specificity rates were greater than or equal to 90% across all organisms tested. Sensitivity and specificity performance results were similar between clinician and patient-collected samples.
In a secondary analysis comparing the performance of NAAT and physician diagnosis within the clinical trial, the Aptima NAAT assays had higher sensitivity and specificity rates than clinicians’ diagnoses and in-clinic assessments across almost all pathogens, indicating that NAAT assays more accurately identify vaginitis pathogens than traditional diagnostic methods. All testing—NAAT and microscopy—had specificity rates of greater than 95% for trichomoniasis detection.
The BD Max multiplex NAAT platform was FDA-approved as an IVD in 2017.2,6 Among BV tested organisms are lactobacilli (Lactobacillus crispatus and L. jensenii) as well as G. vaginalis, A. vaginae, Megasphaera Type 1, and bacterial vaginosis-associated bacterium-2 (BVAB2). CV testing is identified by detection of a Candida group (C. albicans, C. tropicalis, C. parapsilosis, and C. dubliniensis) or C. glabrata or C. krusei, and trichomoniasis is identified by detection of trichomonad protozoa.
To validate this assay performance a cross-sectional study was conducted including 1,740 women with symptoms of vaginitis.6 The objective of the trial was to evaluate the clinical accuracy of the BD Max investigational test for vaginal swabs collected by clinicians or by patients. Patients were all 18 years of age or older. The reference methods for bacterial vaginosis, used for comparison, were Nugent’s score and Amsel’s criteria for intermediate Nugent results. The reference methods for Candida infection were isolation of any potential Candida microorganisms from inoculation of two culture media: chromogenic and Sabouraud agar and sequencing. The reference methods for trichomoniasis were wet mount and culture.
The NAAT test sensitivity, compared with reference methods, was greater than 90% for clinician-collected samples for BV, Candida group, and TV (Table 1). The NAAT test specificity rate was 85.8% for clinician-collected samples for BV. For the Candida group and Trichomoniasis testing, the specificity rate was greater than or equal to 94%. Similar sensitivity and specificity performance results were obtained for clinician- and patient-
collected samples.

Molecular-based NAAT tests using vaginal swabs collected by clinicians or patients can accurately diagnose the most common bacterial, fungal, and protozoan vaginitis infections. The NAAT assays offer sensitive and specific detection of vaginitis and provide accurate diagnoses of multiple pathogens, an advance over prior vaginitis testing methods. These tests provide objective tools for the clinician to differentiate among vaginitis pathogens to confidently diagnose and treat patients. Effective treatment and cure of vaginitis reduces risk of recurrent or persistent infections, helps prevent consequences of untreated infections, and reduces spread of certain STIs. l
Oluwatosin Goje, MD, MSCR, is an obstetrician gynecologist who specializes in the evaluation, diagnostic testing, and management of obstetric and gynecologic infectious diseases. She is an assistant professor of Ob-Gyn and Reproductive Biology at the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University and on staff in the Obstetrics, Gynecology and Women’s Health Institute at the Cleveland Clinic. She leads the Gynecologic Infectious diseases and Vulvar and Vaginal Disorders Centers in the Institute of Obstetrics, Gynecology and Women’s Health Institute. Goje has published and presented locally and nationally on infectious diseases in women.
References
1. Hologic, Inc. FDA Clearance of Aptima BV and Aptima CV/TV Molecular Assays Ushers in New Era of Comprehensive and Objective Diagnostic Testing for Vaginitis. Press Release. May 29, 2019. Available at https://investors.hologic.com/press-releases/press-release-details/2019/FDA-Clearance-of-Aptima-BV-and-Aptima-CVTV-Molecular-Assays-Ushers-in-New-Era-of-Comprehensive-and-Objective-Diagnostic-Testing-for-Vaginitis/default.aspx. Accessed September 16, 2020.
2. Becton, Dickinson and Company. BD MAX Vaginal Panel Receives FDA Market Authorization to Detect Most Common Causes of Vaginal Infections. Press Release. October 21. 2016. Available at https://www.prnewswire.com/news-releases/bd-max-vaginal-panel-receives-fda-market-authorization-to-detect-most-common-causes-of-vaginal-infections-300353885.html. Accessed September 16, 2020
3. Coleman JS, Gaydos CA. Molecular diagnosis of bacterial vaginosis: an update. J Clin Microbiol. 2018;5:e00342–318.
4. Paladine HL, Desai UA. Vaginitis: diagnosis and treatment. Am Fam Physician. 2018;97:321–329.
5. ACOG Committee on Practice Bulletins—Gynecology. ACOG Practice Bulletin. Clinical management guidelines for obstetrician-gynecologists, Number 215, January 2020: Vaginitis in Nonpregnant Patients. Obstet Gynecol. 2020;135:1195–1206.
6. Gaydos CA, Beqaj S, Schwebke JR, et al. Clinical validation of a test for the diagnosis of vaginitis. Obstet Gynecol. 2017;130:181–189.
7. Bacterial Vaginosis (BV) Statistics. Centers for Disease Control and Prevention. Available at https://www.cdc.gov/std/bv/stats.htm. Accessed September 14, 2020.
8. Jeanmonod R, Jeanmonod D. Vaginal Candidiasis (Vulvovaginal Candidiasis) Updated August 16, 2020. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459317/. Accessed September 14, 2020.
9. Vulvovaginal Candidiasis. Centers for Disease Control and Prevention. Available at https://www.cdc.gov/std/tg2015/candidiasis.htm. Accessed September 14, 2020.
10. Larsen B, Monif GR. Understanding the bacterial flora of the female genital tract. Clin Infect Dis. 2001;32:e69–e77.
11. Sobel JD, Subramanian C, Foxman B, Fairfax M, Gygax SE. Mixed vaginitis-more than coinfection and with therapeutic implications. Curr Infect Dis Rep. 2013;15:104–108.
12. Schwebke JR, Gaydos CA, Nyirjesy P, Paradis S, Kodsi S, Cooper CK. Diagnostic performance of a molecular test versus clinician assessment of vaginitis. J Clin Microbiol. 2018;56:e00252–18.
13. Tumietto F, Posteraro B, Sanguinetti M. Looking for appropriateness in the cure of mixed vaginitis: the role of fenticonazole as an empiric treatment. Future Microbiol. 2019;14:1349–1355.
14. Hainer BL, Gibson MV. Vaginitis. Am Fam Physician. 2011;83:807–815.
15. Schwebke JR, Taylor SN, Ackerman R, et al. Clinical validation of the Aptima bacterial vaginosis and Aptima candida/trichomonas vaginitis assays: results from a prospective multicenter clinical study. J Clin Microbiol. 2020;58:e01643–19.
16. Hillier SL, Austin M, Macio I, Meyn LA, Badway D, Beigi R. Diagnosis and treatment of vaginal discharge syndromes in community practice settings. Epub. April 20, 2020. Clin Infect Dis. 2020;ciaa260. doi:10.1093/cid/ciaa260.
17. Mania-Pramanik J, Kerkar SC, Salvi VS. Bacterial vaginosis: a cause of infertility? Int J STD AIDS. 2009;20:778–781.
18. Obiero J, Rulisa S, Ogongo P,Wiysonge CS. Nifuratel-Nystatin combination for the treatment of mixed infections of bacterial vaginosis, vulvovaginal candidiasis, and trichomonal vaginitis. Cochrane Database Syst Rev. 2018;4. doi:10.1002/14651858.CD013012.
19. Sobel JD. Syndromic treatment of women with vulvovaginal symptoms in the United States: A call to action! Epub. April 30, 2020. Clin Infect Dis. 2020;ciaa267.
20. Chavoustie SE, Eder SE, Koltun WD, et al. Experts explore the state of bacterial vaginosis and the unmet needs facing women and providers. Int J Gynaecol Obstet. 2017;137:107–109.
Featured image: Trichomonas vaginalis protozoan, illustration courtesy Dreamstime.





Great web site you have here.. It’s hard to find high-quality writing like yours these days. I truly appreciate individuals like you! Take care!!