POC testing is unlocking new markets for commercial IVDs, but reaching potential new customers can be a challenge.
By Kate McLaughlin, PhD, and Donna Hochberg, PhD
Diagnostic testing that is capable of being performed at the point of care holds the potential to improve patient care by enabling faster clinical decisions with small sample volumes. New instrument platforms are addressing historic concerns over quality and data integrity to allow a wider variety of tests to be performed outside of the lab. At the same time, new models of more-convenient healthcare delivery, and the prospect of capturing additional revenue by performing tests for which lab proficiency testing and inspections are waived under the terms of the Clinical Laboratory Improvement Amendments of 1988 (CLIA), are together giving physicians, pharmacists, and nurses more power to shift testing volume to the point of care.
Still, commercialization of point-of-care (POC) technologies remains challenging for manufacturers, and lab-governed organizations must adapt to the workflow implications of POC testing. While there is no one-size-fits-all approach, a better understanding of the technological and clinical trends driving decentralized and POC testing can help ensure commercial success for manufacturers and enable labs to seamlessly integrate POC capabilities.
Broadened Availability
Existing models that guide when, where, and how healthcare services are delivered—including diagnostic testing—are being reshaped by increasing consumer empowerment, mounting cost pressures, and technological evolution. In this changing world, transporting samples for centralized analysis at hospitals and reference centers remains operationally efficient for labs, but can lead to inefficient clinical workflows that fall short of the convenience that physicians and patients are coming to expect.
POC testing offers an alternative approach, enabling physicians and patients to review results and determine the best course of action within a continuous episode of care. Unlike common lab instrumentation, POC platforms are rapid (sample to answer in 15 minutes or less), low throughput (possibly one sample at a time), small (often handheld or less than one cubic foot in size), and user-friendly (with simple menus and ready-to-use packaged consumables). These features substantially reduce the burden of user training, calibration, and documentation, and permit testing to be performed in settings outside of a certified lab, such as clinics, pharmacies, the hospital bedside, or even a patient’s home.
For healthcare providers, the ability to assume a more active role in caring for patients, minimize callbacks to discuss lab results, and capture reimbursement for these tests can be compelling drivers of interest in POC testing—so long as staff have sufficient bandwidth to take on a new activity and workflow. In acute-care settings, POC testing can enable critical decisions to be more rapid and data-driven, improving outcomes. Patients also stand to benefit from the convenience of a single appointment and the potential to replace some venipunctures with fingersticks.
For hospital labs, POC testing offers the possibility of addressing clinician demands for faster results, but carries the risks of increased test utilization and greater direct costs for consumables. Furthermore, labs face the additional responsibility of overseeing the performance and documentation of POC tests performed in clinical care areas of the hospital. Thus, the decision process for offering a test at the point of care must analyze on a case-by-case basis the offsetting advantages of efficient high-throughput centralized testing and the clinical benefits of obtaining test results more rapidly (see “The Impact of Routine POC Testing“).
Expanded Capabilities
The range of disciplines and use cases for which POC testing is a suitable option has expanded dramatically over the past decade, driven by advances in detection technologies and electronics (see Figure 1). Lateral-flow tests and dipsticks remain in common use for drugs of abuse, infectious diseases, pregnancy, and urine chemistry, but their limited sensitivity and qualitative nature make such methods poorly suited to more-complex analytes or critical assays.
More recently developed POC platforms apply on a smaller scale the same principles as high-throughput core lab instruments, and many are capable of executing complex protocols that include centrifugation, washing, and multiple reagent incubations in a self-contained disposable format (see Table 1). Such capabilities allow platforms such as the FastPack system by Qualigen, Carlsbad, Calif, to detect hormones (see Figure 2), and the Io system from Atlas Genetics, Trowbridge, UK, to perform molecular tests for sexually transmitted and hospital-acquired infections, with sensitivity and specificity comparable to larger platforms. Sysmex America, Lincolnshire, Ill, recently achieved a milestone in the field of POC testing by receiving a CLIA waiver for performing a complete blood count on the company’s new XW-100 system (see Figure 3). While the complete blood count is one of the most commonly ordered tests, complex operating principles and interpretation of its many parameters have long relegated it to licensed labs. Sysmex overcame these barriers in part by simplifying the results to a three-part differential and 12 total parameters.
Cutting-edge POC instruments are capable of multidisciplinary testing, including capabilities for performing hematology, immunoassay, and molecular tests. The SpinIt platform by Biosurfit, Lisbon, Portugal, employs CD-like cartridges to perform a complete blood count with five-part differential, and to test for C-reactive protein (CRP) and hemoglobin A1c (HbA1c). The SearchLight system under development at FluxErgy, Irvine, Calif, promises to integrate chemistry, hematology, immunoassay, and molecular testing on a single low-cost instrument.
In the near future, more POC systems will be designed to perform tests using multiple technologies, or will utilize such new detection methods as label-free surface plasmon resonance and piezoelectric detection to perform an increasingly broad panel of assays using a single sample and consumable (see Figure 4).
Getting Connected
Data connectivity is another key feature of the latest generation of POC instruments. Historically, the need to manually capture the results of lateral-flow tests in the patient’s medical record placed a considerable burden on office staff. The need to reduce such uses of staff time has prompted the advent of dedicated lateral-flow readers such as the Veritor Plus by Becton Dickinson (BD), Franklin Lakes, NJ (see Figure 5). Like Veritor, most newer instruments come standard with user lockout and Ethernet or Wi-Fi connections, enabling them to export results directly to a laboratory information system (LIS) or electronic health record (EHR).
For some POC instruments, labs and equipment vendors can review performance from a central dashboard, simplifying maintenance, consumables inventory, and documentation. Some platforms designed for use in the developing world, such as the GeneXpert Omni system by Cepheid, Sunnyvale, Calif, take this a step further, and can use cellular networks to collect data in a Cloud-based archive for remote analysis. The broad use of POC testing for infectious diseases can support real-time epidemiological analysis and reporting of outbreaks at the community level, as shown with the Idylla Connect capability offered by Biocartis, Mechelen, Belgium. Such an effort would not be possible under centralized testing models and can help shorten the time to recognition and control of outbreaks, slashing transmission rates.1
Stakeholder Buy-In
In hospital settings, agreement among clinicians, hospital management, and lab personnel is critical for the successful adoption and expansion of POC testing. Nurses, physicians, medical assistants, and other ‘front-line’ users of POC tests can be powerful advocates for decentralized testing. But to overcome their resistance to changing established processes, they must see a tangible benefit to their own workflow (such as closing a case or evaluation sooner) or to patient outcomes (such as a faster change in the course of care). Conversely, processes that add to the already heavy workload of clinical staff (such as leaving the bedside to bring a sample to an instrument) can be deal breakers.

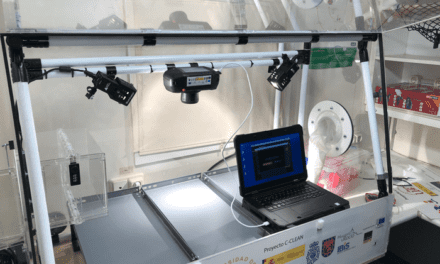
Figure 4. Major in vitro diagnostic manufacturers that offer point-of-care diagnostic systems, by technology type.
For hospital finance and purchasing departments, the higher direct costs of POC testing can be a substantial issue. However, a detailed analysis of staffing allocation, patient flow, and compliance with accreditation guidelines for rapid turnaround of some tests, such as troponin, can help to justify this investment.
As labs are ultimately responsible for the quality and documentation of all diagnostic testing at the hospital, regardless of where and how the test is performed, they also have a strong voice in this decision—including the selection of specific technologies and products. Features such as onboard calibration and data connectivity, discussed earlier, can reduce the burden on labs and help ensure compliance. Nevertheless, labs must also address the challenges of ensuring comparability between results measured at the point of care and on lab instrumentation, and training end-users on the new instruments, both of which may require a substantial investment of resources until a POC test becomes well established.
Many other healthcare delivery sites lack an onsite lab—for example, physician offices, nursing homes, and pharmacies—and have traditionally relied on reference labs and hospital outreach programs to provide phlebotomy and testing services. Today, these settings are ripe for greater use of POC testing, enabled by the broader menu and diversity of platforms available in CLIA-waived formats. Adoption can be driven by a customer service orientation (for instance, providing an influenza or respiratory syncytial virus result during a pediatric visit rather than calling the concerned parent back), workflow improvements (minimizing the burden of callbacks and enabling doctors to close one case and move on to the next), and the potential to increase profitability by opening new revenue streams.2 The menu of desired POC tests in such settings is also different from those needed in hospitals, and far less driven by the urgency of the result itself. Improving the convenience of routine tests such as cholesterol or lead can improve patient compliance with recommendations and enhance the patient-doctor relationship.
Busy physician offices rely on rapid turnover of exam rooms, and strongly prefer instruments that can give a result within the scheduled visit duration. The space required for the instrument and a reasonable inventory of consumables can also present challenges for smaller offices, especially if the consumables are large or require refrigeration.

Figure 6. Potential benefits of point-of-care testing systems for healthcare providers and patients.
Clinics at pharmacies and retail stores play a growing role in delivering acute care for common ailments. Offering POC tests is not only well aligned with the priorities of their convenience-minded patients but also creates a captive audience for the primary retail business. In this context, the pressure on turnaround time is not as great, making cost and ease of use the more important criteria when selecting an instrument. Unlike hospital staff, staff in these settings commonly lack phlebotomy skills, and alternative sample types such as fingersticks or swabs are strongly preferred.
For companies developing and marketing POC testing systems, these market dynamics present both challenges and opportunities (see Figure 6). Instrument features, turnaround time, and sample-handling workflows all influence the ideal customers and use cases for each technology. The complex interplay among these factors means that companies with a novel technology and visions of developing POC applications will find no simple, one-size-fits-all approach for building a compelling menu or targeting customers.
Reaching Customers
Understanding customer expectations for the physical form and size of POC systems is key to optimally meeting their needs, and can inform a callpoint-focused approach to the market. Benchtop-format instruments, such as the microwave-sized FastPack immunoassay system by Qualigen, can be convenient for office-based specialists to place in a central location. But such large instruments would not be attractive for use in busy emergency departments or neonatal intensive care units, where space is at a premium and leaving the bedside to carry the sample to the unit is discouraged. In such settings, hospital staff generally prefer handheld and portable units such as the Minicare I-20 instrument for troponin testing by Philips Healthcare, Amsterdam (see Figure 7).
While any POC system can provide results faster than a reference lab, many office-based practices see no meaningful difference between receiving test results in 30 minutes or receiving them in 12 hours. Nevertheless, technologies capable of providing results in 10 minutes or less—such as traditional lateral-flow formats or newer rapid quantitative immunoassay systems—reduce callbacks and reflex testing, and are most convenient for patients.
Such new CLIA-waivable molecular systems as the Cobas Liat analyzer by Roche Diagnostics, Indianapolis (see Figure 8), and the Alere i analyzer by Alere, Waltham, Mass (see Figure 9), offer results in as little as 15 minutes and provide immediately actionable test results for infectious diseases such as influenza and respiratory syncytial virus. Molecular systems with longer turnaround times can demonstrate their value in other ways: the Idylla system by Biocartis, Jersey City, NJ, empowers oncology clinics to perform molecular tumor profiling in less than 2 hours; while the FilmArray system by BioFire Diagnostics, Salt Lake City, offers a more-extensive syndromic workup for infectious diseases (see Figure 10).
Because FDA will not grant CLIA-waived status to instruments that require the users to centrifuge or manually manipulate a patient sample, many POC systems use whole blood samples. However, the tasks of obtaining and loading small volumes of blood present a different set of problems for end-users. For capillary samples, questions remain about the comparability of some analytes to reference values from venipuncture. The lack of a capillary blood collection protocol that is standardized across instruments can also lead to errors—such as not wiping away the initial drops of blood, or milking the finger—and can produce inaccurate test results due to the variability of the sample itself or differences in the normal analyte concentration between venous and capillary samples.3 Loading the sample in the test consumable often requires the use of a transfer pipette, and is a process that can be messy and prone to error. Issues such as these can present considerable barriers to implementing POC testing.
In response, some in vitro diagnostics (IVD) companies are developing simpler alternatives, such as using capillary action to draw the sample directly from fingertip to the consumable. Thinking beyond the technical details of the test itself to ensure a smooth sample-to-answer workflow demonstrates an appreciation for customers’ needs and can be a key differentiator in an increasingly competitive market.
As POC testing unlocks new markets for commercial IVDs, reaching these potential new customers can also be a challenge. Many companies with innovative POC systems are based around a technology rather than a clinical need, reflecting the companies’ relatively limited experience with current IVD testing workflows and end-user expectations. These companies also tend to be small and independent, unlike the companies that supply most core lab equipment, with limited resources for sales and marketing.
Furthermore, the geographic distribution and diversity of potential customers is much greater for POC technologies than for core labs. While there are only about 5,000 registered acute care hospitals in the United States, there are tens of thousands of primary care practices, and roughly 10,000 independent clinics that perform testing for office-based specialty practices. These customer groups are further fragmented by size, case mix, current testing workflows, available labor, and financial health—all factors that can affect interest in POC testing in general as well as the specialist’s desired features for POC systems. Establishing a relationship with prospective POC testing customers is a challenge, even for established IVD companies such as bioMérieux and Cepheid, which are well known to laboratorians, but not to physicians.
Conclusion
After a long incubation, the field of POC testing is now developing rapidly as new technologies mature, healthcare delivery models evolve, and societal expectations for rapid results challenge the traditional centralized lab paradigm. The benefits that POC testing can hold for clinicians and patients will continue to increase the volume and diversity of tests performed.
Labs will be instrumental in this transition, as judicious institutional gatekeepers and experienced advisors for new user types. A deeper understanding among stakeholders—including labs, clinicians, health system management, and diagnostics companies—will help ensure that the features, clinical applications, and settings of POC testing are all aligned with the common goal of improving patient care.
Donna Hochberg, PhD, is a partner and leads the diagnostics and life science tools practice, and Kate McLaughlin, PhD, is a vice president and spearheads the life science research tools practice, at Health Advances, Weston, Mass. For further information, contact CLP chief editor Steve Halasey via [email protected].
References
- Perkins MD, Dye C, Balasegaram M, et al. Diagnostic preparedness for infectious disease outbreaks. Lancet. Epub ahead of print, 31 May 2017; doi: 10.1016/S0140-6736(17)31224-2.
- Lewandrowski EL, Yeh S, Baron J, Crocker JB, Lewandrowski K. Implementation of point-of-care testing in a general internal medicine practice: a confirmation study. Clin Chim Acta. 2017;473:71–74; doi: 10.1016/j.cca.2017.08.019.
- Tang R, Yang H, Choi JR, et al. Capillary blood for point-of-care testing. Crit Rev Clin Lab Sci. 2017;54(5):294–308; doi: 10.1080/10408363.2017.1343796.