Using current standard human epidermal growth factor receptor 2 (HER2) assays as a diagnostic test may result in a mis-assignment for treatment of breast cancer with a promising new drug, according to a new study from the Yale Cancer Center.
The study analyzed current assays used to determine the effectiveness of treatment for patients with breast cancer using trastuzumab deruxtecan (T-DXd). The findings were published online in JAMA Oncology.
“The results suggest that a new test should be developed to ensure that the right patients are offered T-DXd. Using the current assay, as many as 50 percent of patients thought to respond to the drug may not respond,” says senior study author David Rimm, MD, PhD, Anthony N. Brady Professor of Pathology and Director of Yale Pathology Tissue Services at the Yale Cancer Center. “The poor assay performance also gives the pathologist a bad image in that it appears they are unable to distinguish a positive from a negative test. However, the problem is not the accuracy of the pathologists, it is the mis-match of an old test with a new drug.”
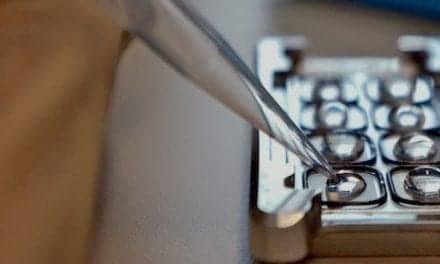
The current IHC test is used to derive a score that measures the amount of HER2 proteins on the surface of cells in a breast cancer tissue sample. T-DXd is currently being tested in large, randomized trials with registration intent for this patient population.
T-DXd is showing great efficacy in patients with breast cancer with HER2 immunohistochemistry (IHC) scores of 1+ or 2+, but not with a score of 0, as read in central pathology labs, according to Rimm and colleagues.
In this study, researchers collected data from the College of American Pathologists (CAP) survey and an assessment of analytic data from a Yale-based study of concordance of 18 pathologists reading 170 breast cancer biopsies. CAP surveys showed 19% of the cases read by 1400 labs generated results with less than 70% agreement between a HER2 score of 0 vs 1+.
In a second part of the study, when 18 pathologists read the same slides from a selected set of breast cancer biopsies using a four-point scale, there was only 26% agreement amongst pathologists on scores of 0 and 1+due to the poor quality of the current test in the critical range for the new drug T-DXd.
“We plan on developing a new diagnostic assay for T-DXd to help improve accuracy of selection for treat treatment for this new breast cancer drug,” says Rimm. “We also hope to better define the threshold to determine which patients will benefit, and which will not in the new test.”
Funding for this study was provided by The Breast Cancer Research Foundation and the National Cancer Institute. Aileen I. Fernandez, PhD, is lead author of the study. Other Yale scientists contributing to this research include: Matthew Liu, Malini Harigopal, MD, and Lajos Pusztai, MD, DPhil.
Featured image: David Rimm, MD, PhD, Anthony N. Brady Professor of Pathology and Director of Yale Pathology Tissue Services at the Yale Cancer Center. Photo: Yale Cancer Center