A recent database analysis reveals that in recent years, sexual minority individuals—those whose sexual orientation differs from societal norms—were less likely to have undergone cervical cancer screening tests than heterosexual counterparts.
The study also observed that Hispanic sexual minority individuals had the lowest screening rates. The findings are published by Wiley online in CANCER, a peer-reviewed journal of the American Cancer Society
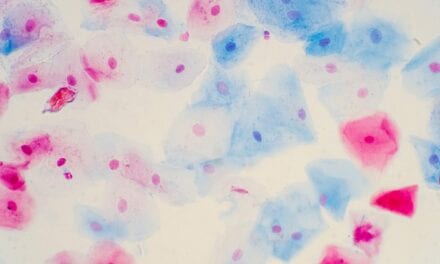
Regular Pap tests are recommended for those with a cervix who are aged 21 to 65 years old to detect cervical cancer at premalignant or early stages, when treatments are most effective. Numerous barriers to cervical cancer screening exist, and for sexual minority people, these may include inadequate patient-provider communication, mistrust in medical providers, fear of discrimination in the clinic, and the belief that Pap testing is not beneficial.
Investigators analyzed 2015–2018 data from the National Health Interview Survey—an interview-based program that collects information from U.S. households on a broad range of health topics—to examine cervical cancer screening disparities related to individuals’ self-defined sexual minority status and race/ethnicity.
The team found that sexual minority individuals had 46% lower odds of ever undergoing Pap testing compared with heterosexual persons. When the intersection of sexual orientation and race/ethnicity was considered, white sexual minority participants and Hispanic sexual minority participants had reduced odds of ever undergoing Pap testing compared with white heterosexual participants. No significant differences were observed between white heterosexual participants and participants of Black sexual minority or Hispanic heterosexual identities.
“This research highlights the need to examine disparities at the intersection of multiple societally constructed identities. More work is needed to alleviate disparities, and future work should incorporate measures of systemic discrimination,” says lead author Ashley E. Stenzel, PhD, of Allina Health, a not-for-profit health care system based in Minneapolis, Minnesota.
An accompanying editorial notes that campaigns addressing patient knowledge and provider communication may help to improve screening rates, and that cultural adaptation of interventions is needed to reduce existing disparities.