Introduced as the COVID-19 pandemic took hold, the triage approach offers women and labs a more efficient and effective way to diagnose and manage cervical cancer earlier, improving long-term survival rates.
By Chris Wolski
As the U.S. returns to a semblance of “normalcy” after almost three years of living under the cloud of the COVID-19 pandemic, there has been renewed focus on routine health screenings—including for various types of reproductive cancers.
Focus on cervical cancer screening, in particular, has seen increased interest from clinicians and policymakers.
CLP recently spoke to Karla Loken, DO, OBGYN, FAACOG, the disease area partner for Obstetrics and Gynecology at Roche Diagnostics, about the factors that have led to the increased emphasis on cervical cancer screening, new concepts for diagnosis and monitoring the disease, what better testing regimens will mean for women and their health, and how labs will become more efficient and effective in testing for cervical-cancer-causing conditions, including HPV.
Loken was the Da Vinci Surgical instructor and director of the Joshua Max Simon OB/GYN clinic at St. Vincent Hospital, and has been an adjunct faculty at Marion University Medical School in Indianapolis. She also serves on the board of the Indiana Vaccine Coalition, and has worked in adverse event reporting in oncology, pharma, and clinical development for surgical devices prior to transitioning to her role in medical affairs at Roche.
Answers have been edited for length and clarity.
CLP: It seems that there’s been quite a push for women to be screened for cervical cancer. What do you think is driving this? Is it just a consequence of our returning to so-called normalcy after two-plus years dealing with the COVID-19 pandemic or is there some other factor driving this?
Karla Loken: There’s a couple of reasons. First, many people have put off cancer screenings during the pandemic. A recent JAMA article noted that cervical cancer screenings are down by 11%. Also, better technology has developed over the past few years that allows us to detect cancer earlier. And we know that when detected at an early stage, the 5-year survival rate for women with invasive cervical cancer is 92%.
CLP: My understanding is that most tests for HPV have good sensitivity, but may not have as good specificity—how does that impact women and their health?
Loken: That’s true, HPV tests lead to a good indication of who is at risk for developing disease. The next step–specificity–is finding out who has precancerous changes.
CLP: One concept that I think is very intriguing is the triage testing that Roche introduced in 2020. Can you explain that to me a bit more and why it could help cut cervical cancer deaths?
Loken: Yes, we are motivated by the fact that earlier detection can save lives. OBGYNs and lab professionals have shared with us that better screening and diagnostic methods related to HPV could change their ability to fight against cervical cancer and provide better outcomes for patients.
Cervical cancer is primarily caused by HPV, and about 80% of men and women will have had an HPV infection by age 45.[1] While most people exposed to HPV do not develop cervical cancer, advanced medical testing is necessary to determine who is most at risk and will benefit from more immediate follow-up and who is at lower risk and should be given more time to clear the infection and retested sooner. It is especially important to identify when HPV infection is transforming as early as possible because only about four in 10 women come back for the later testing.[2]
The Roche Cervical Cancer portfolio is made of the following three FDA-approved tests:
- The cobas HPV Test can accurately identify if a patient is at risk of cervical cancer
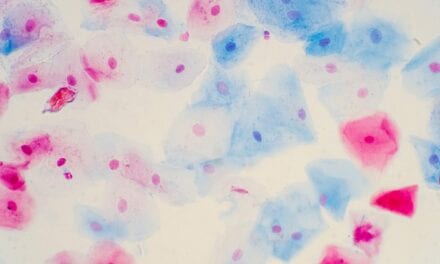
- The CINtec PLUS Cytology determines if the patient is progressing toward cervical cancer
- CINtec Histology confirms the presence or absence of cervical precancer
The cobas HPV Test, used in primary screening, checks for 14 types of high-risk HPV genotypes in cervical cancer. It includes results for HPV 16, HPV 18 and 12 other pooled.
The portfolio also includes the FDA-approved dual stain biomarker to determine if a patient is progressing to cervical cancer.[3] CINtec PLUS Cytology allows clinicians to detect a person’s pre-cancer earlier and is a technical innovation similar to how advances in mammography have given clinicians the ability to detect disease earlier.
In the IMPACT clinical trial, co-testing and primary screening with CINtec PLUS Cytology as a triage detected cervical disease earlier in seven out of 10 women who were already identified as HPV positive.[4]
CLP: Does the triage approach help labs be more efficient?
Loken: Yes, adding this step reduces the number of unindicated colposcopies, which occupy time and technical expertise for the lab analyzing the tissue sample.
CLP: Is cervical cancer one of the cancers that is being addressed by the Cancer Moonshot program? If so, in what way? And why is it important to do so?
Loken: The Cancer Moonshot program calls out that there are certain cancers that can be eliminated, with cervical cancer being one of them. This brings a national focus and combined effort of research and industry to solve this issue.
CLP: What will better cervical cancer screening—co-testing, triage, better specificity, etc.—mean for women’s health long term? Will we ever see a time when cervical cancer joins the ranks of colon cancer in that it is a very treatable, survivable disease?
Loken: It is very possible to eliminate cervical cancer through screening, vaccination, and early testing. Cervical cancer was once the leading cause of cancer death among people with a cervix. However, it is the most preventable of all gynecologic cancers. In the past 40 years, the number of cases of and deaths from cervical cancer have decreased significantly as more women regularly had Pap tests. The introduction of human papillomavirus or HPV testing further enhanced our ability to detect those at risk. Working together, we can eliminate cervical cancer.
Chris Wolski is chief editor of CLP.
References
[1] Chesson HW, Dunne EF, Hariri S, Markowitz LE. The Estimated Lifetime Probability of Acquiring Human Papillomavirus in the United States. Sex Transm Dis. 2014;41(11):660–4.
[2] Rebolj and Lynge, Br J Cancer, 2010 103(3)
[3] Wright TC Jr, Stoler MH, Ranger-Moore J, Fang Q, Volkir P, Safaeian M, Ridder R. Clinical validation of p16/Ki-67 dual-stained cytology triage of HPV-positive women: Results from the IMPACT trial. Int J Cancer. 2021 Sep 18. doi: 10.1002/ijc.33812. Online ahead of print.
[4] Wright TC Jr, Stoler MH, Ranger-Moore J, Fang Q, Volkir P, Safaeian M, Ridder R. Clinical validation of p16/Ki-67 dual-stained cytology triage of HPV-positive women: Results from the IMPACT trial. Int J Cancer. 2021 Sep 18. doi: 10.1002/ijc.33812. Online ahead of print