by Gary Tufel
Qualified histotechnicians/histotechnologists: Why the shortage, why it’s unique, what’s being done to remedy it
The histology profession is facing serious challenges, according to Carrie Diamond, executive director, National Society for Histotechnology (NSH), Columbia, Md. The aging workforce is making it difficult to find qualified histotechnology staff, she says, and there are several causes.
First, schools are closing due to lack of funding and the expense of running histology programs. The lack of public awareness for the discipline, coupled with the industry’s pay scale, have made it increasingly more difficult to attract people into the profession. Salaries for histology technicians tend to be lower than other lab disciplines, because histology technicians’ educational requirements do not require a 4-year degree. In addition, the onslaught of new digital and molecular technologies, as well as new standards, being adopted by the industry require additional training for techs, but this training is becoming increasingly difficult to acquire due to the lack of funding for continuing education, Diamond says.
It is, and has been for the past 5-plus years, extremely difficult to find trained, certified histotechnicians and histotechnologists, agrees William DeSalvo, BS, HTL (ASCP), Quality Control Committee chair, NSH, and system production manager, Sonora Quest Laboratories, Tempe, Ariz. “There is a steady exit of older technologists, and we have no real coordinated effort/system/program to train and replace,” he says. “The changes confronting the histology laboratory, such as incorporation of higher-complexity testing and the need to personalize patient diagnosis, is demanding that the level of ability and competency for testing personnel be drastically raised and magnifies the deficiencies present in staffing levels and education/training.”
Additionally, DeSalvo says, the pathologist is not as engaged and participatory in the education and training of the histotechnician/histotechnologist. More often than not, there is expectancy that all testing personnel will be able to self-learn, comprehend, and competently perform new techniques and technologies. This is just not happening, he says; instead, there is a knowledge gap being created and too few histotechnologists are available to execute complex testing, let alone have time to train others to become competent.
DeSalvo says there continues to be many students who can move into the field without a defined secondary education, coordinated theory education, or practical training, even though there are several accredited schools. These programs can be as little as 9 months for a certificate and often do not have the space, money, time, or personnel to properly train and provide hands-on practical/technical training, which is absolutely necessary to become a functional and competent performing member of a histology lab.

The Slide Staining Tray for IHC procedures from Newcomer Supply, designed for refrigerator to incubator (-20°C to +70°C), is available in 10-, 20-, and 30-slide capacity units with either a clear or black lid.
The need remains to have functional student bench techs, able to produce the highest-quality work in a productive manner from the very first day they start working in the histology lab. Today’s histology laboratory requires the histotechnician/histotechnologist to spend up to 80% of his or her workday on manual and repetitious tasks because there is a lack of automation.
“There has been a great improvement in semiautomation, staining instruments for routine, special, and immunohistochemistry, but today we still have to process, embed, and cut tissue samples to produce the necessary slide/testing platform needed for more complex testing,” DeSalvo says. “Changing this dynamic is not possible as long as we have a dysfunctional education and training process, which I believe is slowing the development and incorporation of automation.
“I believe we need to emulate the medical technologist or medical laboratory scientist education and training process to help histotechnology move to a more respected, professional, and reliable workforce,” DeSalvo adds. “We need individuals [who] have a defined and specific educational requirement and an extended practical training period, in a working histology laboratory, so that we can actually realize a benefit from supporting and participating in the education and training process of the increasing number of students required to keep the histology laboratory fully staffed. We need a reorganization of the education and training process and the full support of the pathologist, CAP (the College of American Pathologists), and our technical professional societies, ASCP (the American Society of Clinical Pathologists), and NSH.”
DeSalvo notes that the histology laboratory is transforming rapidly with the addition of new technical instrumentation and techniques. “This transformation will stall and falter if we do not create a new partnership with the pathologist and create an environment where we have the ability to discuss issues, exchange information, and develop processes that further affect the patient outcome, improving patient care,” he says. “We cannot progress our professional development while the current state of personnel have extreme diversity in education, training, and knowledge. It is time to recreate the education and training program for the histotechnologist or we will become less relevant in the patient care process.”
FRONT-OF-MIND ISSUES FOR HISTOTECHNICIANS?/?HISTOTECHNOLOGISTS
In digital pathology, in today’s histology laboratory, most would say that automated quantitation and scoring of the amount of expression the breast cancer-associated antigens estrogen (ER), progesterone (PgR), and HER2Nue (Her2) has been the area where most labs start their participation in digital pathology. This process has an increased reimbursement for both the technical and professional component paid by the government and insurance companies.
However, DeSalvo says, this is only the surface of digital pathology. Once this portion has been brought into the histology laboratory, there can then follow expansion of digital pathology to whole slide scanning of other tissue slides/sections to facilitate telepathology, consultation, workflow, and ultimately, increased information, through algorithmic evaluations, to provide more details-differential diagnosis.
“This entire technical area is in a state of flux,” DeSalvo says. “The FDA has stepped in and required that the instruments’ systems, software, and hardware must be thoroughly evaluated before they can be used in the clinical setting. Primary diagnosis cannot be developed through the use of a digital image. Digital pathology has the opportunity to help create results, a stained slide that can be readily shared and compared lab to lab, pathologist to pathologist, and algorithm to algorithm, and reduce the costly repetition of patient testing now taking place in anatomic pathology.”

Newcomer Supply’s BCL-2 ONCOPROTEIN QC slides are used to verify histological techniques and reagent reactivity.*
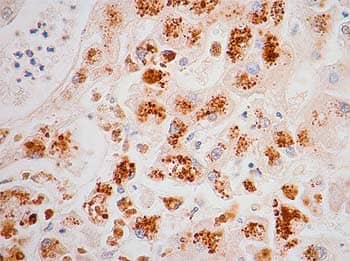
Newcomer Supply’s Hepatitis C Positive Control Slide for IHC is available in 10 or 98 sets.*
Photos courtesy of? NEWCOMER SUPPLY
He notes that there are many obstacles to using, expanding, and relying on digital pathology, including a lack of standardization of tissue sample preparation in the histology laboratory; a lack of training, knowledge, and understanding of the entire process by the practitioners, histotechnician/histotechnologist, and pathologist. Successfully implementing digital pathology in the histology lab is integral to expanding molecular (FISH) testing and the many visualization derivatives. There is a push to incorporate more molecular testing performed in the histology lab to support the further differentiation of patient diagnosis.
The facilitator of the digital and molecular process will, and must be, the histotechnologist, he says. “Again, the progression of this technology points out the education and training deficiencies, and demands the continued improvement of the histotechnologist. The digital pathology, whole-slide scanning, and evaluation is a time-consuming process that, if properly handled by the histotechnologist, will create more productivity and efficiency by the pathologist—in essence, creating more information and more time for the pathologist to develop a specific and personalized diagnosis that moves toward providing more prognostic information,” DeSalvo says.
“Actually, it will allow the pathologist to become more involved in the assessment of the clinical outcome of many types of tumors and be more active in selecting appropriate therapies,” he says. “Digital and molecular pathology make it possible for the pathologist to become a key participatory member in a total patient care process. To attain this new participation level, the histotechnologist must be trained and retrained, and it must be now.”
Not only must there be intense training, but there must be a discussion of true standardization of all tissue-preparation processes, incorporating more stringent quality control and quality assurance processes. “The education, training, and competency issues facing histotechnology must be addressed quickly or there will be a necessity to bring the medical technologist into the histology lab to perform this complex testing,” De Salvo says. “I believe this will be a mistake, as histotechnologists are the only testing personnel who fully understand the preparation process and its effects of the variation of results and can effectively work, partner with the pathologist to provide the information and testing results required to make personalized medicine a reality.”
Joe Myers, MS, CT (ASCP) QIHC, senior technical sales specialist, Biocare Medical LLC, Concord, Calif, which distributes products for ImmmunoHistoChemistry (IHC) and in situ hybridization (ISH) procedures; and chair, IHC Resource Group — National Society for Histotechnology, says that one of the primary reasons there is a shortage of qualified techs in the field of histology is that the training that newly minted technologists receive is often inadequate to prepare them for real-world work situations.
“Although there are more histology programs available, they seem to focus primarily on education in the scientific principles of histology, so that students can pass the ASCP certification exams, rather than on more practical matters,” Myers says. “And I believe that the underlying cause of this problem is that the training provided in these academic settings does not, and cannot, provide students with the quantity of block-sectioning and slide-staining that they will likely encounter upon entering the workforce, nor do these programs place enough emphasis on the essential skill of troubleshooting. Another contributing factor is that many of the facilities in which students perform their externships do not, for ‘liability’ reasons, allow students to section exceptionally small or ‘difficult’ specimens or perform ‘advanced’ procedures such as immunohistochemistry and in situ hybridization.”
As far as efforts to address these issues goes, Myers says it has been his experience that many histology programs have begun working with clinical internship sites to obtain additional and more complex specimen material for students to practice on before they embark on their externships. And, despite the growing importance of molecular microscopic methods in the histology lab, it is unlikely that students can be provided with enough education or training in these settings. More often than not, technologists develop these skills once in the workplace, through training provided by IHC/ISH-product vendors, often at these vendors’ facilities rather than in their own labs.
“Undoubtedly, the use of digital image capture and analysis systems and molecular methods continues to increase within the anatomic pathology lab, and will continue to challenge technologists in this field,” Myers says. “I believe that this is the case because many of the individuals [who] currently perform these procedures have not received formal education or training; rather, they were simply ‘thrown into’ these areas—and although they ultimately learned how to perform IHC/ISH procedures and operate slide-scanners with proficiency, they often do not understand the underlying scientific principles and do not troubleshoot effectively.”
As far as efforts to address these challenges go, Myers says that it is incumbent upon current practitioners to work with various scientific/professional societies to develop education/training programs. “A great deal of expertise exists in this field and, with the support of the practicing pathologists, could be transferred to interested individuals,” he says. One such program is the NSH’s annual IHC/ISH Forum, which is designed to provide participants with a comprehensive overview of these techniques. “Another issue to consider here is that, with the proliferation of automated systems for these technologies, some say that the field has been ‘dumbed down.’ It is, therefore, imperative that new technologists be better educated in the underlying science and shown how these procedures can be, and are, performed ‘by hand.'”
*Quality control slides are used to verify histological techniques and reagent reactivity. They are intended for the qualitative purpose of determining positive or negative results, and not to be used for any quantitative purpose.
Gary Tufel is a contributing writer for CLP. For more information, contact Editor Judy O’Rourke, [email protected].